Abstract
Background
Although multiple studies have shown superiority of allogeneic hematopoietic cell transplantation (alloHCT) over autologous hematopoietic cell transplantation (autoHCT) for patients with "high-risk" acute lymphoblastic leukemia (ALL), these findings may be explained, in part, by contamination of the peripheral blood progenitor cell (PBPC) leukapheresis product by residual leukemic cells in patients undergoing autoHCT.
Methods
We retrospectively evaluated minimal residual disease (MRD) via next-generation sequencing (NGS) (Adaptive Biotechnologies, S. San Francisco, CA) in the PBPC leukapheresis products from 32 ALL patients who underwent autoHCT. All patients had "high-risk" ALL, as defined by B-lineage disease with WBC at diagnosis >30,000/uL; high-risk cytogenetics including t(9;22), t(4;11), other 11q23 abnormalities, or monosomy 7; or primary refractory disease.
Peripheral hematopoietic cell mobilization consisted of cytarabine 2000mg/m2 IV every 12 hours (16,000mg/m2 cumulative) concurrent with etoposide 40mg/kg cumulative by continuous IV infusion over 4 days. The autoHCT conditioning consisted of 1320cGy total body irradiation (TBI) given in 11 fractions from day -8 to -5, etoposide 60mg/kg IV on day -4, and cyclophosphamide 100mg/kg IV on day -2. Tyrosine kinase inhibitors (TKI) were allowed for patients with Philadelphia chromosome-positive (Ph+) B-ALL. Seven patients (22%) participated in a multi-institutional trial in which the PBPC graft underwent ex vivo complement-mediatedpurging using monoclonal antibodies against CD9/CD10/CD19/CD20 for patients with B-lineage disease, or against CD2/CD3/CD4/CD5/CD8 for patients with T-lineage disease.
Kaplan-Meier curves were generated using GraphPad Prism (GraphPad Software, La Jolla, CA) and statistical differences assessed via Log-Rank and Wilcoxon analyses, with a p-value of <0.05 considered significant.
Results
Twenty-eight patients (88%) had diagnostic bone marrow samples with quantifiable immunoglobulin or T cell receptor (Ig/TCR) gene rearrangements suitable for MRD quantification in the PBPC collections. Twelve (38%) patients had Ph+ B-ALL, 12 (38%) had Ph-neg B-ALL, and 4 (14%) had T-cell ALL. The majority of patients were male, in first complete remission, and autografted between 2000-2009, with a median age at autoHCT of 32 (range 19-55).
With a median follow-up of 41 months (range 3-217), median relapse-free survival (RFS) and overall survival (OS) for the entire cohort are 3.2 and 4.2 years, respectively. At 5 years post-autoHCT, 42% of patients remain alive and relapse-free.
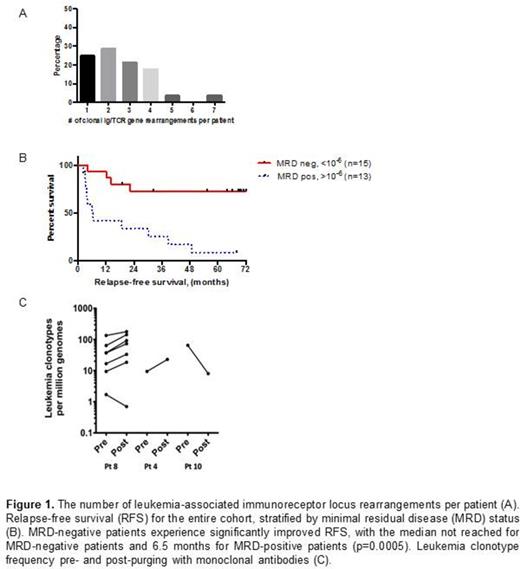
Of the 28 diagnostic bone marrow specimens, 21 (75%) had rearrangements in more than 1 immunoreceptor locus (Figure 1A). A total of 73 rearrangements were identified across all patients. Clonal Ig heavy chain (IGH) sequences with complete VDJ rearrangement were the most commonly identified rearrangement, present in 17 of 28 patients (61%) and representing 30 of the 73 (41%) total rearrangements.
When stratified by graft MRD burden, the median RFS for patients with MRD detectable at a level ≥10-6 (n=13) was 6.5 months, and has not been reached for patients without detectable MRD above this threshold (n=15; p=0.0005; Figure 1B). Ex vivo antibody-based purging failed to eradicate leukemia cells from the PBPC collections of 3 patients with detectable MRD who received a purged graft (Figure 1C), all of whom ultimately relapsed.
Of the Ph+ cohort, 6 (50%) had detectable MRD in the PBPC graft. Two (33%) of these patients were not treated with a TKI; 1 relapsed at 4 months post-autoHCT and the other died from non-relapse mortality. Of the 4 Ph+ patients with detectable MRD who received a TKI, 2 (50%) remain long-term relapse-free survivors. Of the 6 patients without MRD who were treated with a post-autoHCT TKI, 5 (83%) remain relapse-free.
Conclusion
We demonstrate that the NGS-based immunosequencing platform identifies ALL MRD in leukapheresed PBPC collections. The presence of MRD in the autograft strongly predicts relapse, with only 15% RFS in patients harboring ≥10-6 MRD at stem cell collection versus 73% in patients with undetectable MRD. The absence of MRD in PBPC may thus identify a subset of "high-risk" patients likely to achieve long-term remissions without alloHCT. TKI therapy for patients with Ph+ B-ALL may also, in some cases, abrogate the need for alloHCT, even with quantifiable MRD prior to high-dose therapy.
Damon:Atara: Consultancy; Sunesis: Research Funding; Sigma-Tau: Research Funding; McGraw-Hill: Patents & Royalties: Book Chapter. Andreadis:McGraw Hill: Honoraria; Novartis: Consultancy; Cellerant: Consultancy; Pharmacyclics: Honoraria. Olin:Daiichi-Sankyo: Research Funding. Kong:Adaptive Biotechnologies: Employment, Equity Ownership. Faham:Adaptive Biotechnologies: Employment, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal