Abstract
Fanconi anemia (FA) is a rare inherited syndrome characterized by chromosomal instability, eventually resulting in a number of manifestations affecting the hematopoietic system and other organs. The phenotype of FA patients is largely heterogeneous, and encompasses different clinical manifestations that may be present at birth, or rather develop later during the disease course. Thus, even due to the rarity of the disease, the natural history of FA remains hard to be established in its details. To accomplish the need of a large disease registry, in 1994 we have established at the local health unit "ASL Napoli 1" a National Database named as "Registro Italiano Anemia di Fanconi " (RIAF): here we report on a 20-year experience of the Italian FA Registry. Patients were enrolled prospectively at diagnosis or later on, after signature of the informed consent form; epidemiological, genetic and clinical data were recorded at registration, with these latter information eventually collected periodically to assess the clinical course, possible complications and long-term survival. The main endpoint of the study was the description of the natural history, looking for the following variables: family history, disease presentation, development of hematological manifestations, development of malignancies, occurrence of hematopoietic stem cell transplantation (HSCT) and survival. Between 1994 and 2014 a total of 180 patients were included in the RIAF, belonging to 151 distinct families; all diagnoses were based on standard chromosome DEB (diepoxybutane) - or MMC (mytomicin C) - breakage test confirmed at specialized centers. The median age at diagnosis was 3170 days, and it was lower in patients born in the more recent periods; the median follow up of enrolled patient was 15.6 years. For the majority of patients the diagnosis was suspected based on the typical morphological abnormalities and/or growth retardation; congenital abnormalities (mostly skin pigmentation and skeletal abnormalities) were demonstrated in 90% of patients. The majority of patients (77%) exhibited some hematological abnormalities at diagnosis, which in most cases was a mild-to-moderate cytopenia. Looking at the subsequent disease course, a total of 172 (96%) FA patients developed some hematological manifestations, typically progressive cytopenia due to bone marrow failure. The cumulative incidences (CI) of any hematological disorder were 62%, 88% and 94% at 10, 20 and 30 years, respectively, whereas those of a hematological malignancy were 5%, 8% and 22% at 10, 20 and 30 years. Hematological manifestations led to an allogeneic hematopoietic stem cell transplantation (HSCT) in more than half of the patients (57%), with a CI of HSCT of 33%, 64% and 72%% at 10, 20 and 30 years, respectively; patients born in the most recent years were transplanted earlier. The presence at diagnosis of a solid tumor was quite rare; nevertheless, solid tumors were the most significant complication in the long-term period, with a CI of 1%, 15% and 32% at 10, 20 and 30 years respectively; head and neck were the most common cancer sites. Eighty-eight of the 180 FA patients enrolled in the RIAF died during their follow up; in non-transplanted patients, the main causes of death were related to the underlying disease (infections, bleeding, and solid tumors), whereas in transplanted patients graft versus host disease and other transplant-related complications played a major role. The median survival of this large cohort was 22.5 years; overall survival at 10, 20 and 30 years were 88%, 56% and 37%, respectively, with no improvement over the past decades. These data confirm the poor long-term prognosis of FA patients, irrespective of earlier diagnosis and improved treatment options achieved in the most recent years.
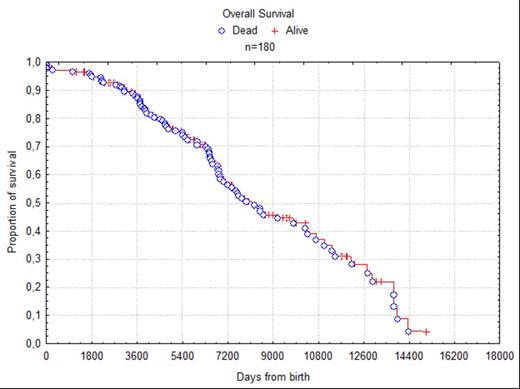
Overall survival of the 180 patients enrolled in the RIAF
Overall survival of the 180 patients enrolled in the RIAF
Risitano:Alexion Pharmaceuticals: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Alnylam: Consultancy, Research Funding; Rapharma: Consultancy, Research Funding; Novartis: Research Funding; Pfizer: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal