Abstract
Introduction: Extracorporeal photopheresis (ECP) is an effective therapy for patients with acute or chronic graft-versus-host disease (GVHD) who have significant skin involvement. During ECP, buffy coat is collected from the peripheral blood (PBL), mixed with 8-methoxypsoralen (8-MOP), and exposed to ultraviolet-A (UVA). Photo-activated 8-MOP crosslinks DNA in nucleated cells, which are infused back to the patient to induce an immune modulatory effect. The exact mechanism of ECP and the optimal cellular dose to treat are unknown. We previously demonstrated a linear relationship between lymphocyte counts in the PBL and the buffy coat, with the collection efficiency affected primarily by the type of ECP machine used (UVAR or CELLEX; Therakos, West Chester, PA). It is therefore feasible to track the cellular dose of ECP by measuring the lymphocyte count in the PBL prior to each procedure. Another outstanding question is whether ECP can be successfully performed at a decreased hematocrit, which is a common finding among patients with GVHD. Due to concerns over the collection efficiency and patient safety, our protocol recommends transfusion of red cells prior to ECP when a patient's hematocrit is in the range of 28-30%. However, there is no evidence from human subjects supporting the relevance of this specific threshold. In this study, we compared the collection efficiency during ECP in GVHD patients with hematocrits between 24% and 29% and those with hematocrits of 29% or higher.
Methods: Patients with GVHD and hematocrits between 24% and 29% were prospectively recruited for this study which was approved by the institutional review board (n=26). The hematocrit of 24% approximated the red cell transfusion threshold for our transplant patient population. One ECP procedure was performed for each patient using the CELLEX with 1500 mL of whole blood processed. PBL was drawn within 24 hours prior to the procedure for a complete cell count with automated differentials. At the end of cell collection but prior to 8-MOP treatment, 1 mL of well-mixed buffy coat was drawn for the complete cell count. Spearman correlation coefficient was calculated for the counts of each nucleated cell type, including neutrophils, lymphocytes and monocytes, in the PBL versus the buffy coat. The collection efficiency, or fold enrichment, was evaluated using the ratio of lymphocyte count in the buffy coat to that in the PBL. The ratio was then compared among the current cohort (lower-hct-CELLEX group) and two historical control groups with hematocrits of 29% or higher who were treated with either UVAR (higher-hct-UVAR group n=6) or CELLEX (higher-hct-CELLEX group, n=16). Mann-Whitney test was performed with a double-sided p value of 0.05. Data visualization and statistical analysis were performed using Prism 6.
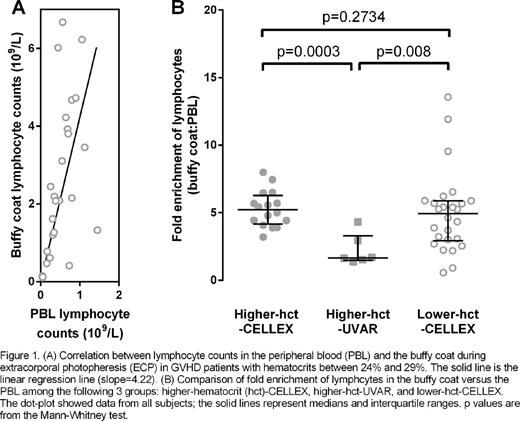
Results: Consistent with our previous findings in patients with higher hematocrits, there was a significant correlation between lymphocyte counts in the PBL and the buffy coat in the lower-hematocrit-CELLEX group (r=0.66, p=0.0002) (Figure 1A). A significant correlation was also observed for monocytes (r=0.46, p=0.02) but not neutrophils (r=0.26, p=0.20). The distribution of lymphocyte counts was fit into a linear regression model with a slope of 4.22 (95% CI: 3.06-5.37, p < 0.0001). The fold enrichment for lymphocytes was higher in the lower-hct-CELLEX group than in the higher-hct-UVAR group (medians: 4.94 versus 1.66, p=0.008). The fold enrichment for lymphocytes was not significantly different between the lower-hct-CELLEX group and the higher-hct-CELLEX group (medians: 4.94 versus 5.22, p=0.27) (Figure 1B). According to previous protocols, approximately 1-2 units of red blood cells would have been transfused for each patient in the lower-hct-CELLEX group prior to each procedure. These transfusions were completely avoided without any adverse events observed throughout the study.
Conclusions: The fold enrichment of lymphocytes during ECP using the CELLEX is comparable between GVHD patients with hematocrits between 24% and 29% and patients with hematocrits of 29% or higher. Unnecessary red blood cell transfusion may be avoided without significant increase in adverse events. The efficacy and safety of this practice warrant further investigation in a larger cohort.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal