Abstract
Context: Cirrhosis impacts the coagulation cascade since the first stage of the liver disease. For years, a procoagulant imbalance, related to the severity of cirrhosis, has been demonstrated. This procoagulant imbalance is detected when coagulation assays are sensibilised to the protein C pathway. A resistance to thrombomodulin (TM) is consistently found in thrombin generation assays. TM and endothelial protein C receptor (EPCR) are two transmembrane proteins involved in the anticoagulant protein C pathway. A soluble form of EPCR (sEPCR) is release of the endothelial surface upon cleavage by mettaloprotease. Soluble EPCR have a procoagulant and proinflammatory effects: bound to PC or activated PC (APC), PC is unavailable for activation by thrombin-TM complex and APC is unable to inactivate FVa and FVIIIa. The aim of this study was to evaluate the plasma levels of sEPCR in non-complicated cirrhotic patients as a potential marker for procoagulant imbalance, compared to healthy controls.
Materials and Methods: Patients prospectively included were confirmed cirrhotic patients (prothrombin time <70% and/or liver dysmorphia and/or fibroscan > 20 kPa and/or histology and/or association of portal hypertension and liver failure). Patients were free of hepatocellular carcinoma and were not anticoagulated. Patients with on-going infection or inflammatory complication were excluded. None of them had a thromboembolic event or a familial history of thromboembolism. Controls were free of anticoagulation, coagulation disorders and without oral contraceptives. All ethical requirments were obtained and patients and controls gave their written informed consent. Kruskal-Wallis test and Dunn post test were used for statistical analysis. Results are expressed as mean (Q1 - Q3) values of sEPCR.
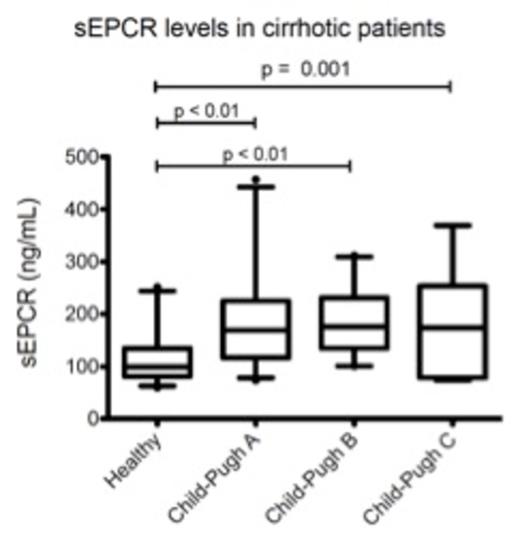
Results: Fifty two cirrhotic patients (24 Child-Pugh A, 21 Child-Pugh B and 7 Child-Pugh C) and 32 healthy controls were prospectively included in our hospital. The sEPCR values for healthy controls were 100 ng/mL (81 - 135 ng/mL). Comparatively to controls, Child-Pugh A patients and Child-Pugh B patients had statistically significant higher values of sEPCR : 169 ng/mL (117-225 ng/mL, p < 0.01) and 176 (135 - 230 ng/mL, p < 0.001) respectively (Figure 1). Compared to healthy controls, Child-Pugh C patients had an increased level of sEPCR : 174 ng/mL (78 - 254 ng/mL, not significant but probably underpowered). These data are in lines with the thrombin generation profiles showing a resistance to TM in cirrhotic patients increasing from Child-Pugh A to C. No patient have developed thrombosis during the follow-up period.
Conclusion: Patients with Child-Pugh A and B cirrhosis had significantly higher values of sEPCR compared to healthy controls (p < 0.01 for both). The putative role of sEPCR as a marker of the procoagulant imbalance associated to cirrhosis remains to be accurately evaluated.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal