Abstract
Diabetic foot infections have a 15-25% lifetime incidence in diabetics, and account for more than half of all non-traumatic lower extremity amputations. Currently, the most accurate means of non-invasively diagnosing osteomyelitis in patients with foot infections is with gadolinium-enhanced MRI. However, gadolinium has limited specificity, as it not only enhances infection but also neuropathic changes and other forms of sterile inflammation. Also, safety concerns about gadolinium have recently been raised given the recent discovery that gadolinium (a molecule that some animal studies suggest is a neurotoxin) deposits in the brains in some patients with normal renal function. Making the correct diagnosis of osteomyelitis is paramount, as an MRI that is falsely positive for osteomyelitis may lead to unnecessary bone biopsies, prolonged antibiotic courses, or even amputation. Ferumoxytol is a superparamagnetic iron oxide nanoparticle (SPION) that is FDA approved for iron replacement in patients with chronic kidney disease. Ferumoxytol is also widely studied as a contrast agent for MRI imaging. Ferumoxytol is taken up by macrophages, and thus provides contrast in areas of active infection, manifested as negative enhancement (eg hypo-enhancement) on T2/T2* sequences. In this prospective feasibility study, ferumoxytol was used as an MRI contrast agent in patients with osteomyelitis.
We included non-septic patients with suspected osteomyelitis who had a baseline MRI using standard sequences. Patients without a contra-indication to gadolinium also were imaged with standard T1 sequences after gadolinium administration. Ferumoxytol was then administered, and ferumoxytol contrasted images were then obtained 12-24 hours after ferumoxytol infusion. When available, resected tissue was analyzed for iron content and macrophages by immunohistochemistry.
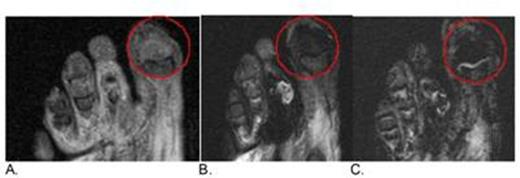
To date we have enrolled 8 patients with possible osteomyelitis. Because this was a feasibility study, statistical analysis is not meaningful in this small cohort of patients. Two patients had strong contrast-enhanced evidence of osteomyelitis on both gadolinium and ferumoxytol imaging. Osteomyelitis was confirmed by histology of the amputated digits for both patients. Representative images from a patient with biopsy confirmed osteomyelitis is shown in Figure 1. Another patient had images that did not demonstrate hypo-enhancement on ferumoxytol imaging, but did have evidence of osteomyelitis on gadolinium-enhanced imaging. This patient underwent an amputation after antibiotics failed to heal this patient's wound, and the pathology came back negative for osteomyelitis. Five other patients did not have tissue available as a reference standard with which to analyze the accuracy of the ferumoxytol enhanced images.
In conclusion, macrophage imaging using ferumoxytol-contrasted MRI merits further study for use in the diagnosis of osteomyelitis.
Patient with 1st distal phalanx osteomyelitis. STIR T2 weighted image precontrast (A), STIR T2 weighted image approximately 16 hours post-ferumoxytol (B), and Heme weighted T2* image (C.) about 16 hours post ferumoxytol showing hypo-enhancement in areas of macrophage iron uptake in distal 1st phalanx in the post-ferumoxytol scans.
Patient with 1st distal phalanx osteomyelitis. STIR T2 weighted image precontrast (A), STIR T2 weighted image approximately 16 hours post-ferumoxytol (B), and Heme weighted T2* image (C.) about 16 hours post ferumoxytol showing hypo-enhancement in areas of macrophage iron uptake in distal 1st phalanx in the post-ferumoxytol scans.
Off Label Use: ferraheme is for iron replacement, and we are using it as a contrast agent..
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal