Increasingly, clinicians are obtaining molecular genetic tests when evaluating patients with unexplained cytopenias. In this issue of Blood, Kwok et al and Cargo et al describe results of mutation testing in 2 series of patients with nondiagnostic marrows. These reports raise an important question: if a clonal mutation is discovered, yet diagnostic criteria for a hematologic neoplasm are not met, what is the diagnosis?1,2
Hematologists learn early in training how to evaluate patients with cytopenias, and this remains a core task of hematology clinical practice. But when common cytopenia-inducing causes (eg, vitamin or essential mineral deficiency, infection, immune dysregulation, drug effect, bleeding, organ dysfunction, neoplasia) have been systematically excluded, yet cytopenias persist, clinicians may be puzzled and patients left feeling unsettled. The term “idiopathic cytopenias of undetermined significance” (ICUS), a frank admission of pathophysiological ignorance, has been proposed to describe such patients.3
ICUS includes a hodgepodge of conditions. By definition, patients with ICUS are not known to have a clonal hematopoietic disorder. Some people with ICUS will spontaneously recover normal hematopoiesis, others will eventually be diagnosed with a nonhematologic disease, and a few will turn out to have myelodysplastic syndromes (MDS), especially older patients.
Because morphologically dysplastic cells are common in the marrow of healthy people older than 50 years of age,4 detection of mild dysplasia is not enough to diagnose MDS, even in a cytopenic patient. Instead, in order for MDS to be diagnosed according to World Health Organization (WHO) criteria, patients must exhibit either extensive cellular dysplasia, an increase in marrow blast proportion, or an MDS-associated karyotypic abnormality.5 Long-term natural history studies of large ICUS cohorts are lacking, so we cannot yet counsel patients with ICUS about their risk of developing MDS, acute myeloid leukemia (AML), or another hematologic neoplasm.
Enter mutation testing. More and more, academic institutions and commercial pathology laboratories are offering clinicians the opportunity to test their cytopenic patients for gene mutations commonly associated with hematologic neoplasms. Given the high frequency of such mutations in patients with bona fide MDS,6 it would be easy to label cytopenic patients with mutations but without other findings as having MDS, or at least a disease state similar MDS.
But recent data indicate that at least 10% of patients older than 70 years of age have clonal mutations detectable at a variant allele frequency (VAF) of ≥2%.7,8 We have termed this state, “clonal hematopoiesis of indeterminate potential” (CHIP).9 Like the parallel precursor conditions monoclonal gammopathy of undetermined significance (MGUS) and monoclonal B-cell lymphocytosis, CHIP confers a risk of subsequent diagnosis of overt hematologic malignancy of 0.5% to 1% per year, and CHIP is associated with increased all-cause mortality. The presence of mutations in apparently healthy people with normal blood counts should give the astute clinician pause before assuming cytopenia plus mutation is equivalent to MDS.
The articles in this issue help define the relationship between ICUS, CHIP, and MDS. Using conventional hematopathology techniques supplemented by a 22-gene panel, Kwok and colleagues prospectively analyzed 144 patients with unexplained cytopenias whose samples were sent to a large commercial pathology laboratory for diagnostic testing.1 Although 17% of cases met criteria for MDS, 15% had ICUS with mild dysplasia and 69% had ICUS without dysplasia; thus, ICUS was fivefold more common than MDS. Mutations were detected in 71% of MDS, 62% of ICUS with dysplasia, and 20% of ICUS without dysplasia; the frequency of mutations in the latter group is still higher than that for the general population.
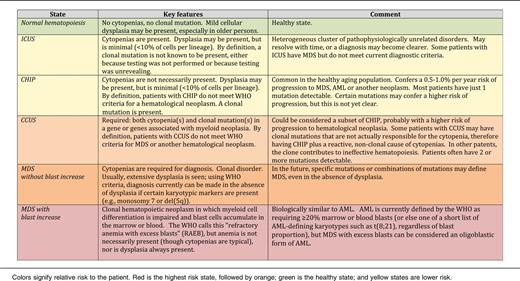
The authors then confirmed these findings in a comparison of 91 lower-risk MDS (79% mutation rate) and 249 ICUS (45% mutation rate in cases with dysplasia, 17% without dysplasia), and proposed the term “clonal cytopenias of undetermined significance” (CCUS) to describe ICUS accompanied by a clonal mutation (see table). The most common mutations observed in the CCUS population included DNMT3A, TET2, ASXL1, and TP53, similar to CHIP. SF3B1, in contrast, was overrepresented in MDS compared with ICUS/CCUS/CHIP, probably because of the strong association of SF3B1 mutations with the morphologic hallmark of ring sideroblasts.10 Unfortunately, follow-up data on these ICUS/CCUS patients is not available.
Cargo and colleagues, from a large regional hematology service in the United Kingdom, looked at this diagnostic challenge from another direction. Using a 26-gene MiSeq assay, the investigators assessed 69 patients who developed MDS or AML who had previously undergone a nondiagnostic marrow.2 This group represented 1.7% of 4835 patients referred to the service over an 8-year period for evaluation of unexplained cytopenias. The investigators found that 91% of these patients had mutations detectable in the nondiagnostic sample: a higher rate than in the series by Kwok et al. Unfortunately, the number of nondiagnostic samples with mutations among patients who did not progress to MDS or AML is unknown. Although most patients with CHIP have only 1 detectable mutation and VAF is often <10%,7 64% of patients in the Cargo series had 2 or more mutations and the median VAF was 40%, suggesting they were at higher risk of subsequent hematologic neoplasia evolution.
It is clear that some individuals with clonal mutations, cytopenias, or both develop MDS, whereas most others do not. A critical next step will be to conduct longitudinal studies of cohorts of ICUS and CCUS. Eventually, we may come to understand that patients with certain mutations or combinations of mutations have a natural history equivalent to MDS, such that they should be considered to have MDS despite the absence of morphologic dysplasia or a karyotypic abnormality. Other mutations may turn out to be less consequential, just as most elderly men with acquired loss of the Y chromosome do not have MDS or another disorder, even though clonal cells from MDS patients may have a −Y karyotype.11
In addition, mutation testing at the DNA level does not tell the whole story, and clinicians will need to learn how to use results from RNA-Seq and assays of epigenetic marks or other biomarkers. Eventually, it will also be possible to abort an emerging clonal process before it evolves to MDS or AML, thereby practicing a form of preventive hematology. Until then, the declaration of doubt inherent in words such as “uncertain” and “indeterminate” will remain a fundamental part of the definitions of ICUS, CHIP, and CCUS.
Conflict-of-interest disclosure: D.P.S. consulted for Genoptix in 2014 and has unrelated technology (an erythropoiesis stimulating agent hemodialysis dosing algorithm) licensed to Mayo Clinic Ventures, which is affiliated with Mayo Medical Laboratories.