Abstract
Background: According to the WHO classification, secondary acute myeloid leukemia (s-AML) includes cases occurring in patients (pts) receiving prior antineoplastic treatments as well as cases developing in pts with a history of previous hematology disorders, such as a myelodysplastic syndrome (MDS) or a chronic myeloproliferative disease (MPD).
Outcomes for this large group of pts, which has a high median age and a high frequency of unfavourable cytogenetics, has been traditionally considered very poor, compared to AML developing “de novo”, and treatment with intensive chemotherapy (iCT) is not standardized in elderly pts. Indeed pts with s-AML have been excluded from molecular and cytogenetic prognostic stratification defined by the ELN criteria.
Aim: Since patients with s-AML actually represent an heterogeneous subgroup of pts a multicenter retrospective study was performed to analyse their outcome in relationship to age, fitness and ELN risk stratification, in order to potentially identify subgroups at different prognosis.
Patients and Methods: We evaluated 127 pts, representing 35% of a population-based series of elderly AML, aged > 65 years (y), diagnosed at five Hematology Centers of the Hematological Network of Lombardy in Northern Italy from January 2008 to May 2014. Thirteen pts (10%) had t-AML and 114 (90%) had AML secondary to previous hematological disorders (89 MDS and 25 MPD). Median age was 74 y (range 65-94 y). Performance status (PS) was evaluable in 122 pts (96%) and PS ECOG was >3 in 32 pts (26%). According to “fitness criteria”, (Ferrara et al, Leukemia, 2013), 126 pts (99%) were evaluable: 54 pts (42.5%) were fit to i-CT (FIT), 55 (43.3%) unfit to i-CT (UNFIT), 17 (13.4%) unfit to ni-CT (FRAIL). Intensive CT was given to 34 (27%), ni-CT (low-dose arac, azacytidine or experimental non-myelotoxic drugs) to 26 (20%) and best supportive care (BSC) to 67 pts (53%). Overall concordance between the fitness and the treatment actually received was 78%.The ELN prognostic criteria were applicable in 69 pts (54%), because of lack of complete molecular and cytogenetic data in the others. Six pts (8.5%, all NPM1+) were at low, 14 (20%) at intermediate-1, 11 (16%) at intermediate-2 and 38 (55%) at high risk.
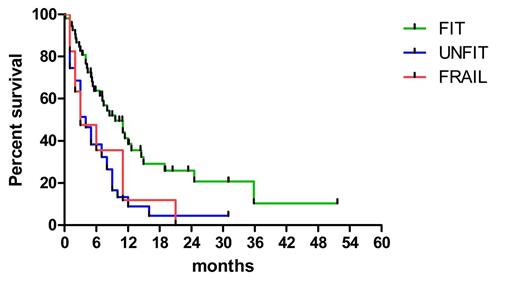
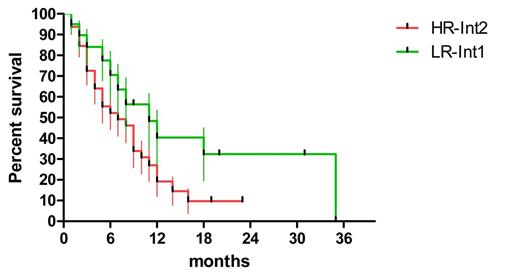
Results: The median OS according to fitness was 9,6, 4 and 3 months (ms), in FIT, UNFIT and FRAIL pts, respectively (p=0.0021) (Figure 1). Both the treatment received (i-CT or ni-CT vs BSC) and the risk ELN classification were related to OS (p< 0.0001 and p=0.0089, respectively). In FIT pts the median OS was 8 ms in pts treated with i-CT, 11 ms with ni-CT, and 3 ms with BSC (p<0.0001) (i-CT vs ni-CT : p=0.6) (Figure2).
The achievement of CR was related to outcome (median OS 12.7 ms vs 5 ms) (p= 0.0035). AML with antecedent hematological disorder (53.8%) or with t-AML (50%) had similar CR rate (53,8% vs 50%) as well as OS (median OS 11 ms vs 7 ms) (p =0.5).
According to ELN risk, OS was better in LR/Int-1/int2 vs HR (median OS 11,4 vs 5 ms, p=0.0035) (Figure 2).
Moreover, also the achievement of CR was related to ELN risk: 100% in LR, 57% in Int1/Int2, 14% in HR (p= 0.012), and percentages differed from de novo AML only in HR pts. Prognosis of the subgroup of 34 ELN low/Int1 risk pts treated with i-CT was fair with CR rate of 53%, and 2 y OS 40% compared to 10% in similarly treated Int2/HR pts (p=0.07).
Conclusion: Elderly pts with s-AML are an heterogeneous subgroup both according to fitness and to ELN risk stratification and these parameters are significantly related to clinical outcome. Overall prognosis of elderly patients with s-AML is not exceedingly worse than in elderly with de novo AML. Outcome was better using i-CT or ni-CT compared to BSC, with no differences between the two treatment modalities. ELN risk stratification merits to be applied also to patients with s-AML and its integration with fitness criteria can identify a subgroup of patients which may benefit from intensive CT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal