Abstract
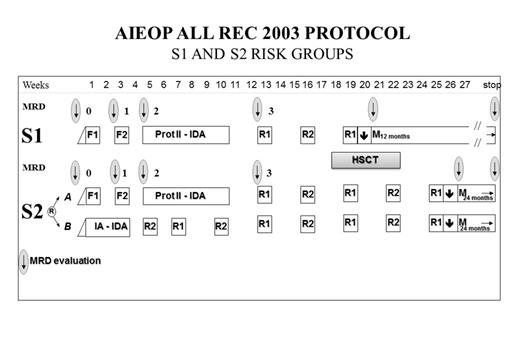
Leukemia recurrence remains the main cause of treatment failure in children with ALL. The prognosis of children with relapsed ALL is strongly influenced by the site of relapse, time elapsing between diagnosis and recurrence and by blast cell immune-phenotype. Recently, several groups reported probabilities of disease-free survival (DFS) in the order of 60% for children with low/intermediate-risk ALL in 1st relapse using different approaches. Despite this remarkable progress, the best re-induction and consolidation treatment remains to be defined. We, thus, conducted from 10/2003 to 06/2012 a multicenter randomized trial aimed at comparatively evaluating the efficacy of 2 alternative approaches in centers affiliated to the Italian AIEOP network. Included in the study were patients below the age of 18 experiencing late (i.e. more than 6 months from treatment discontinuation) isolated extramedullary (IEM) relapse (S1 patients, #22) or children with B-cell precursor (BCP)-ALL who had early (i.e. between 18 months from diagnosis and 6 months after completion of front-line treatment) or late combined bone marrow (BM) relapse, late isolated BM relapse of BCP–ALL, and very early (i.e. within 18 months from diagnosis) or early IEM of either BCP-ALL or T-cell ALL (S2 patients, # 255). S2 children were randomized to receive induction therapy consisting of either two multiagent chemotherapy courses, F1 and F2 (ARM-A), according to the ALL-REZ BFM P95/96 trial, or a classical 4-drug continuous reinduction therapy (protocol I-A-IDA, ARM-B). After induction, ARM-A patients were given a continuous treatment element including idarubicin (Protocol II-IDA), followed by 5 additional alternating R1/R2 courses and maintenance therapy (24 months). After induction therapy, ARM-B patients received 8 additional alternating R1/R2 courses and maintenance therapy (24 months, see Figure 1). S1 patients received ARM-A treatment with the exception of only 3 alternating R1/R2 consolidation courses and shorter maintenance therapy (12 months). All S2 children with an available HLA-identical sibling were candidate to receive allogeneic hematopoietic stem cell transplantation (allo-HSCT), while those relapsing within 48 months from diagnosis were eligible to receive the allograft also from an unrelated donor (UD) of BM cells or a suitable UD cord blood unit. For S1 patients, both autologous (auto) and allo-HSCT were considered acceptable post-remissional options; auto-HSCT was also employed in a minority of S2 children relapsing more than 48 months from diagnosis. Of the whole cohort of children, 143 were males and 134 were females; median age at diagnosis and at time of relapse was 5 (range 0.2-17) and 9 (range 1.1-17.9) years, respectively. Among the 255 S2 patients, 127 were allocated to ARM-A and 128 to ARM-B. All S1 children obtained a 2nd complete remission (CR), while the probability of reaching 2nd CR of S2 patients was similar in the 2 randomization arms (95% vs 96%). The 6-year DFS for the 22 S1 children was 75% (confidence interval, CI, 55-94); 13 of these children were given either auto-HSCT (#7) or allo-HSCT (#6), while 9 were treated with chemotherapy only. The 6-year DFS for the 255 S2 children was 65% (CI 57-72); the DFS for ARM-A and ARM-B patients was 60% (CI 48-71) and 69% (CI 60-79), respectively (p=ns). Among S2 patients, 179 received allo-HSCT either from an HLA-identical sibling (#51) or a BM/CB UD (#105) or an HLA-partially matched relative (#23) after T-cell depletion of the graft (TCD haplo-HSCT). Of the remaining 76 children, 12 were given auto-HSCT, while 64 received chemotherapy only. The 6-year DFS for S2 children who did or did not receive allo-HSCT was 66% (CI 58-74) and 58% (CI 38-77), respectively (p=ns). Among allo-HSCT recipients, the 6-year DFS was 59% (CI 42-75), 72% (CI 62-82) and 62% (CI 41-83) for children given HLA-identical sibling, UD or TCD haplo-HSCT, respectively (p=ns). Altogether, these results confirm that a high proportion of children with low-/intermediate-risk relapsed ALL can be rescued by second line therapy, including transplantation. A re-induction course similar to that employed in first-line therapy is as effective as that proposed in the ALL-REZ BFM P95/96 trial. UD-HSCT and TCD haplo-HSCT are suitable and effective alternatives for children candidate to an allograft but lacking an HLA-identical sibling.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal