Abstract
Background
Patients with myeloproliferative neoplasms (MPNs) are reported to have a higher risk of thrombosis compared to the general population. However, the magnitude of the increase in risk in MPNs patients is not known since there is a lack of studies including control subjects. Therefore, we conducted a large population-based study to assess the risk of arterial and venous thrombosis in patients with MPNs in relation to matched controls.
Patients and Methods
All patients with MPNs reported to the Swedish Cancer Register and/or registered in the Inpatient Register from 1980 to 2009 were included. For each patient, four controls matched for age, sex, and county of residence, were randomly identified from the Register of Total Population. End of follow-up was December 31st 2010.
Events of arterial and venous thrombosis, including deaths, were identified from the Inpatient and Outpatient Registers and the Cause of Death Register. Arterial thrombosis was defined as myocardial infarction, ischemic stroke, or peripheral arterial thrombus/embolus. Venous thrombosis was defined as pulmonary embolism, deep venous thrombosis (DVT), liver or splanchnic vein thrombosis, cerebral venous sinus thrombosis, or other venous thrombosis/embolus.
Odd ratios (ORs) of arterial and venous thrombosis at diagnosis +/-30 days were calculated using logistic regression. Cox regression and flexible parametric models were used to estimate proportional and non-proportional hazard ratios (HRs) with 95% confidence intervals (CIs). Follow-up in all regression models started 30 days after diagnosis to avoid detection bias at time of diagnosis.
Results
A total of 11,155 patients and 44,620 matched controls were identified. Forty-six percent (n=5,161) were men and median age at MPN diagnosis was 69 years.
The OR for arterial and venous thrombosis at time of MPN diagnosis +/- 30 days was 55.0 (95% CI 51.1-59.2 p<0.001) and 64.3 (42.2-98.1 p<0.001) respectively in MPN patients compared to controls.
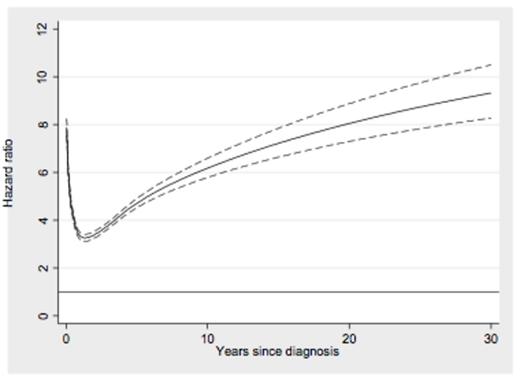
In MPN patients, the risk of arterial thrombosis was significantly 4.9-fold (4.8-5.0 p<0.001) increased compared to matched controls. The HR of myocardial infarction was 3.9 (3.7-4.1 p<0.001) and stroke 4.9 (4.8-5.0 p<0.001) in MPN patients. The HR of arterial thrombosis in MPN patients decreased shortly after diagnosis but thereafter increased with follow-up time in relation to controls (Figure 1a). There was a similar risk of arterial thrombosis in patients of different MPN subtypes compared to controls, the HR in patients with polycythemia vera (PV) was 5.0 (4.8-5.2), essential thrombocythemia (ET) 4.7 (4.6-5.0), primary myelofibrosis (PMF) 5.0 (4.7-5.3), and MPN-unclassifiable (MPN-U) 5.1 (4.8-5.5), respectively.
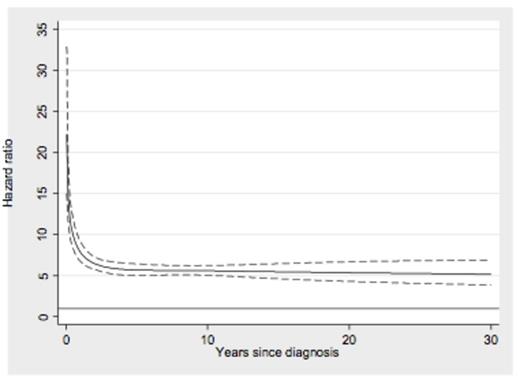
The HR of venous thrombosis in MPN patients was 6.7 (6.2-7.2 p<0.001), where the HRs of pulmonary embolism was 7.5 (6.6-8.5 p<0.001) and DVT was 5.3 (4.8-5.9 p<0.001) compared to matched controls. MPN patients had a substantially increased risk of liver and splanchnic vein thrombosis, HR=41.4 (26.4-64.9 p<0.001). The risk of venous thrombosis in MPN patients decreased shortly after diagnosis and thereafter remained stable in relation to controls during follow-up time (Figure 1b). Compared to controls, patients with PV had a larger increase in risk of venous thrombosis than the other subtypes (HR=9.0; 8.0-10.1), while the HR of venous thrombosis in patients with ET was 5.4 (4.7-6.2), PMF 6.0 (4.9-7.5), and MPN-U 4.6 (3.7-5.7), respectively.
Conclusions
Patients with MPNs have an overall five- to sevenfold elevated risk of thrombosis compared to the general population. The highest HRs were seen for venous thrombosis, especially abdominal thrombosis. The odds of having a thrombosis at time of MPN diagnosis were high, indicating that thrombosis is an important first symptom of MPN. The elevated risk of arterial thrombosis increased while the elevated risk of venous thrombosis remained stable during follow-up time.
This large population-based study is, to our knowledge, the first to quantify the excess risk of thrombosis in MPN patients compared to the general population. Our results indicate that we need to consider time after diagnosis in risk score models and rethink the strategies for thromboprophylaxis in patients with MPN in order to decrease the risk of thrombotic events.
Risk of arterial (a) and venous (b) thrombosis in MPN patients compared to matched controls during follow-up time.
Risk of arterial (a) and venous (b) thrombosis in MPN patients compared to matched controls during follow-up time.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal