Abstract
Introduction
Disparities in clinical care have been described for patients who have limited insurance coverage or social support. We hypothesized that patients with relapsed Hodgkin's lymphoma (HL), non-Hodgkin's lymphoma (NHL), or multiple myeloma (MM) treated at an urban county hospital for whom autologous stem cell transplant (ASCT) was indicated would face barriers for referral to a private academic transplant center, and would have inferior survival compared with similar patients treated primarily at the transplant center. We analyzed a series of patients with HL, NHL, or MM treated at the county hospital and determined referral rates, frequency of ASCT, and overall survival rates compared to similar patients treated primarily at the transplant center.
Methods
Following IRB-approval, charts of consecutive patients with HL (n=39), NHL (n=96), or MM (n=80) treated at Grady Memorial Hospital, a county hospital of Atlanta, between 2007 and 2013 were reviewed. Abstracted data included clinical indication for ASCT by histology (MM patients, and relapsed patients with HL and NHL), reasons for non-referral, decision whether to offer ASCT at the academic center, and survival following referral. Censored data were used to calculate the follow up period for each group. Kaplan-Meier survival plots were generated for subsets of referred patients.
Results
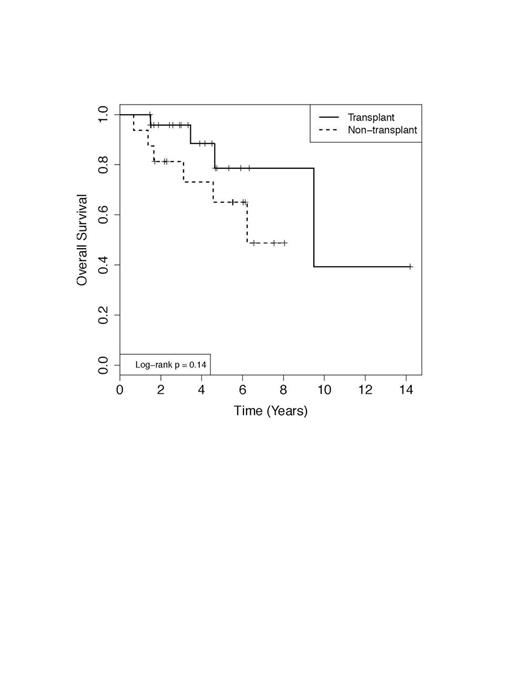
A total of 215 patients with diagnosis of HD, NHL, MM were identified. Information for 12 (6%) patients was not available. The remaining 203 patients constituted the study group. 43 patients were referred for ASCT consults and 160 patients were not referred. Patients not referred for ASCT included: 21 (13%) with Karnofsky performance status (KPS) <60%; 71 (45%) in remission; 16 (10%) with NHL histology in which ASCT is not indicated including newly diagnosed follicular lymphoma, marginal zone lymphoma, peripheral T-cell lymphoma (PTCL), and chronic lymphocytic leukemia; 9 (6%) with refractory disease; 14 (9%) who refused referral, or who lost to follow up, or referred to a VA hospital; 5 (3%) who died before referral; 5 (3%) with age >70 years; 1 (1%) with psychosocial barriers; 6 (4%) who were illegal immigrants; 4 (3%) noncompliant to medical regimens; 2 (1%) with substance abuse; and 1 (1%) lacking adequate social support for ASCT. Among the 43 referred patients, 27 patients were transplanted, 16 were not transplanted. Among transplanted patients, 19 patients had MM, 5 had NHL, and 3 had HL. Reasons for non-transplant included: recommendation to continue conventional maintenance and chemotherapy for MM [n=5 (31%)]; comorbid conditions and KPS <60% [n=4 (25%)]; refractory/progressive diseases [n=4 (25%)]; disease not indicated for ASCT [n=2 (13%)] including PTCL, good response to the current chemotherapy in HL; and noncompliance with treatment [n=1 (6%)]. Two patients in the transplant group were excluded in the analysis of survival due to lack of data on the date of diagnosis. Median follow-up for all referred patients from the time of diagnosis was 4.2 [1.5-14.2] years including a follow-up of 3.3 years [1.5-14.2] in the transplant group, and 5.8 years [1.7-8.0] in non-transplant group. 8-year survival of transplanted patients from the date of diagnosis was 78.6% versus 48.8% for patients not transplanted. (log-rank test, p-value=0.14) (See figure). From the date of ASCT, 8-year survival of transplanted patients was 77.3%. Among transplanted patients, 8-year survival from the date of ASCT was 68.9% for MM patients with no deaths noted to-date in patients with NHL or HL who underwent ASCT. Post-transplant survival among referred patients was not inferior to post-transplant survival among patients treated primarily at the transplant center.
Conclusion
In the era immediately prior to implementation of the Affordable Care Act (ACA), the process of referral of patients with MM, NHL, or HL from a county hospital to an academic tertiary care center for ASCT appeared appropriate, without significant barriers based upon insurance or social support status. Post-referral decisions whether to proceed to ASCT were made based upon established criteria. Post-ASCT survivals among referred patients were comparable or superior to those of patients treated primarily at the transplant center and published series. Further evaluation is needed to assess the impact of the ACA on access to ASCT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal