Abstract
[Background] We have been performing reduced-intensity stem cell transplantation (RIST) to avoid preconditioning-related complications. However, the effectiveness of RIST in pediatric patients with acute lymphoblastic leukemia (ALL) remains to be clarified.
[Methods] We retrospectively reviewed 37 pediatric patients with ALL in second complete remission (CR2) who underwent first allogeneic hematopoietic stem cell transplantation (allo-SCT) between 1993 and 2012 in our institute. We compared the outcomes of RIST with those of myeloablative stem cell transplantation (MAST).
[Results] The median age at allo-SCT was 9 years (range, 1 to 18 years). There were 33 B-lineage ALL, 3 T-lineage ALL, 1 lineage unknown ALL, and none of Philadelphia chromosome-positive ALL. Sixteen patients received HLA-matched bone marrow (7 related; 9 unrelated), 12 HLA-mismatched bone marrow (11 unrelated; 1 HLA haploidentical related), 4 cord blood, and 5 CD34 positive peripheral blood stem cells (HLA haploidentical related). In all patients, the 5-year overall survival (5y-OS) rate and the 5-year event free survival (5y-EFS) rate were 75.1% and 56.5%, respectively.
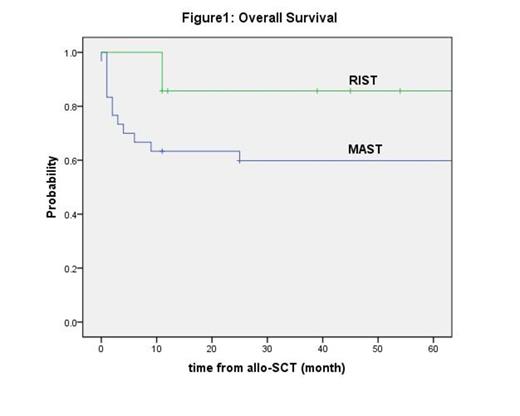
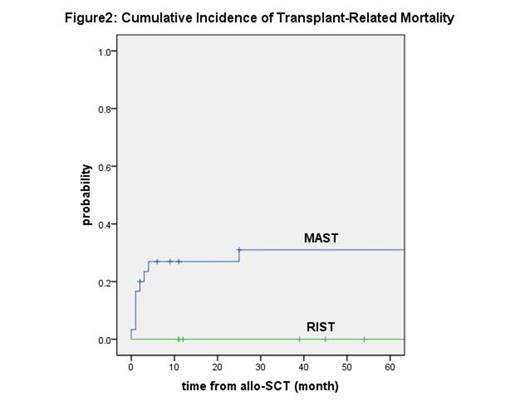
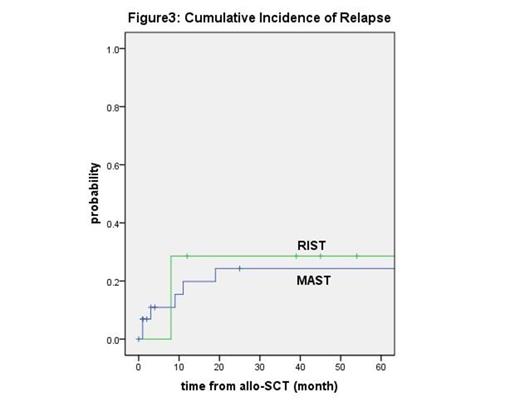
Seven patients underwent RIST and 30 patients underwent MAST. The median follow-up durations of RIST and MAST groups were 3.3 years (range, 0.9 to 8.2 years) and 11.3 years (range, 0 to 21.2 years), respectively. The 5y-OS rates in RIST and MAST groups were 85.7% and 59.8%, and the 5y-EFS rates were 71.4% and 53.3%, respectively. The 5-year cumulative transplant-related mortality (TRM) rates in RIST and MAST groups were 0% and 31.0%, and the 5-year cumulative relapse rates were 28.6% and 24.3%, respectively.
[Discussion] In our series, the cumulative relapse rate in RIST group was similar with that in MAST group, and the cumulative TRM rate in RIST group was lower than that of MAST group. Therefore, both of the 5y-OS and the 5y-EFS rates in RIST group seem to be better than those in MAST group. The outcomes of RIST in our series do not seem to be poorer. Although further studies are needed because of the small size of patients and short follow-up duration, RIST can be considered as the first transplantation for pediatric patients with ALL in CR2.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal