Abstract
Background: Reduced intensity conditioning (RIC) regimens have allowed the use of allogeneic hematopoietic stem cell transplantation (HSCT) in older and high risk individuals, though Graft versus Host Disease (GVHD) remains an issue. Host antigen presenting cells have been implicated in the pathogenesis of GVHD. Extracorporeal photopheresis (ECP) has been shown to modulate host antigen presenting cell function. Tufts Medical Center developed a novel RIC regimen incorporating ECP, pentostatin and reduced dose total body irradiation (PPT). We now report our 14 year experience with this regimen in 206 consecutive patients not eligible for a myeloablative HSCT.
Methods: The Tufts BMT database, the Center for International Bone Marrow Transplantation Registry (CIBMTR) database, and chart review were used to gather data. All patients received a conditioning regimen consisting of ECP administered on days -6 and -5, pentostatin 4mg/m2 by continuous infusion over 48 hours on days -4 and -3, a total dose of 600 cGy TBI administered in 3 fractions on days -2 and -1. No antithymocyte globulin was given. All patients received GVHD prophylaxis with cyclosporine and 2 doses of methotrexate. Supportive care was provided per institutional guidelines.
Overall survival (OS) was calculated from day 0 using the Kaplan Meier method. Cumulative incidence of non-relapse mortality (NRM) was calculated treating death due to primary hematologic malignancy or relapse as competing risks. Univariate associations between patient characteristics and outcomes were estimated using logistic regression or Cox proportional hazards models as appropriate.
Results: 206 patients (56% males) underwent allogeneic HSCT with the PPT regimen between October 1999 and December 2013. Median age at transplant was 53 years (19-70 years) with 45% being older than 55 years. 31% had a prior autologous HSCT. Median time from diagnosis to transplant was 17 months (range 1-180 months). 59% of the transplants were from matched siblings and 41% were from unrelated donors. Marrow was utilized as the source of stem cells in 72% of the transplants. 92% transplants were HLA matched with 8% mismatched at one antigen. The most common indications for transplant were Acute Myelogenous Leukemia (AML) (35%), Myelodysplastic Syndrome (MDS) (16%) and Non-Hodgkin Lymphoma (NHL) (12%). Of the 73 patients with AML 33% were in first complete remission (CR1), 18% were in a second or greater complete remission (CR ≥2) and 49% had active disease at the time of transplant.
Median times to neutrophil and platelet engraftment were 17 and 19 days, respectively. 17% of the patients never dropped their platelet counts below 20,000/mm3.
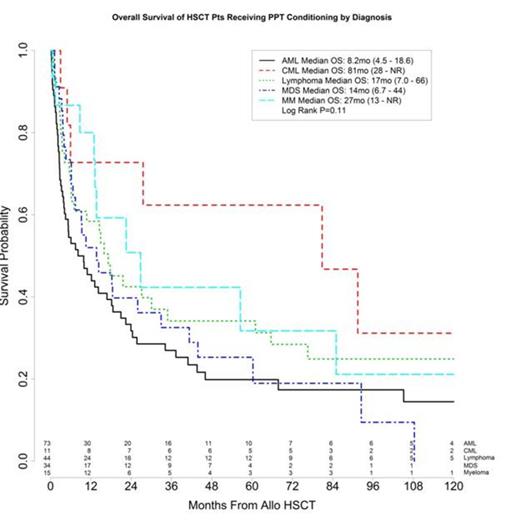
The estimated 5 year overall survival (OS) for the entire cohort was 29% [95% CI (23%-36%)]. The estimates of OS by diagnosis are shown in Figure 1. The estimated non-relapse mortality (NRM) at 100 days was 17% [95% CI (13%-23%)]. The incidence of grade 3-4 acute GVHD was 20%. 54% of the patients developed chronic GVHD, of which only 17% were extensive stage.
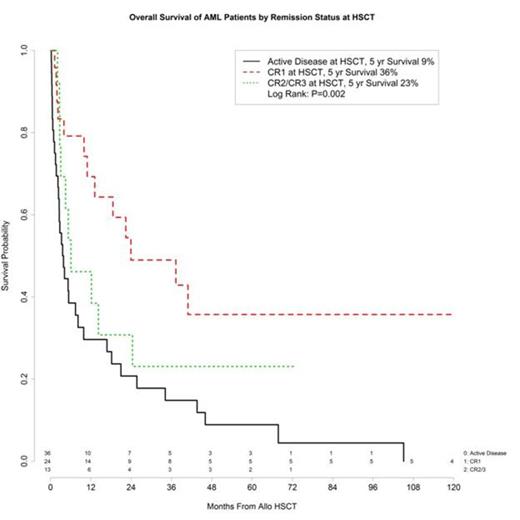
On univariate analysis for the entire cohort, the variables significant for a higher risk of death were 1-antigen mismatch [HR 1.96, p-value=0.01] and KPS <80 [HR 10.66, p-value <0.001]. Age, stem cell source and having an unrelated donor were not found to be significant. On multivariate analysis in the AML cohort, advanced age [aHR 1.37, p-value=0.02] and active disease [aHR 3.02, p-value=0.002] were significant factors for death. OS by remission status in the AML cohort is shown in Figure 2.
Conclusions: PPT was well tolerated with low NRM and survival outcomes comparable to other RIC regimens. OS was independent of graft type (related versus unrelated) or stem cell source. Rates of severe acute and extensive chronic GVHD were low, possibly due to the use of ECP and its modulation of the host antigen presenting cells. OS in patients with AML was comparable to other RIC regimens despite almost half of the patients having active disease at the time of transplant. Our long term follow-up data of 14 years shows that PPT remains a novel regimen for patients not eligible for full intensity conditioning.
Overall Survival of Patients Receiving PPT Conditioning by Diagnosis
Overall Survival of Patients Receiving PPT Conditioning by Diagnosis
Overall Survival of AML Patients by Remission Status.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal