Abstract
Introduction: The optimal stem cell mobilization regimen for patients with multiple myeloma (MM) remains undefined. Most transplant centers use either a chemo-mobilization strategy using cyclophosphamide (CY) and granulocyte-colony stimulating factor (G-CSF) or a steady state strategy using G-CSF alone or with plerixafor in case of mobilization failure. However, very few studies compared efficacy, toxicity and cost-effectiveness of stem cell mobilization with cyclophosphamide (CY) and G-CSF versus G-CSF with preemptive plerixafor. In this study, we retrospectively compared our single center experience at the American University of Beirut in 89 MM patients using fractionated high-dose CY and G-CSF as our past preferred chemo-mobilization strategy in MM patients with our new mobilization strategy using G-CSF plus preemptive plerixafor. The change in practice was implemented when plerixafor became available, in order to avoid CY associated toxicity.
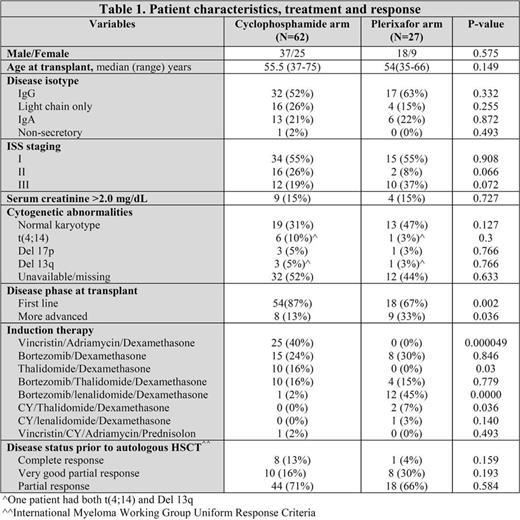
Patients and methods: Patients in the CY group (n=62) (Table 1) received either fractionated high-dose CY (n=56) (5g/m2 divided in 5 doses of 1g/m2 every 3 hours) or CY at 50mg/kg/day for 2 doses (n=6). G-CSF was started on day +6 of chemotherapy at a fixed dose of 300 µg subcutaneously every 12 hours. All patients in the plerixafor group (n=27) (Table 1) received G-CSF at a fixed dose of 300 µg subcutaneously every 12 hours daily for 4 days. On day 5, if peripheral blood CD34+ was ≥ 20/µl, apheresis was started immediately. Plerixafor (240 µg/kg) was given 7-11 hours before the first apheresis if CD34+ cell count on peripheral blood on day 5 was <20/µl and before the second apheresis if CD34+ cells on the first collect were <3х106/kg. The median number of prior therapies was 1 (range: 1-3) in both groups.
Results: Compared with plerixafor, CY use was associated with higher median peak peripheral blood CD34+ counts (35 vs 111 cells/µl, P= 0.000003), and total CD34+ cell yield (7.5 х 106 vs 15.9 х 106 cells/kg, P= 0.003). All patients in both groups collected ≥4x106 CD34+ cells/Kg. Moreover, 60 (96.7%) and 46 (74.2%) patients in the CY group vs 24 (88.8%) and 6 (22%) patients in the plerixafor group collected >6х106 and >10x106 CD34+ cells/kg, respectively (P=0.16; P<0.00001). Only 4 (6.4%) patients required two apheresis sessions in the CY group compared to 11 (40%) in the plerixafor group (P=0.0001). Conversely, CY use was associated with higher frequency of febrile neutropenia (60% vs 0%; P<0.00001), blood transfusions (27% vs 0%; P<0.00001), platelets transfusion (25% vs 0%; P<0.00001) and hospitalizations (64% vs 0%; P<0.00001). No one required intensive level of care and all recovered. Autografting was successfully performed in all patients using high-dose melphalan with a median time from mobilization to the first transplant of 31 days (range: 16-156) in the CY group compared to 13 days (range: 8-40) in the plerixafor group (P=0.027); and median infused CD34+ cells were 7х106/kg (range: 3.1-15.3) versus 5.27 (2.6-7.45), respectively (P=0.002). The average total cost of mobilization using the adjusted costs based on National Social Security Fund (NSSF) prices in Lebanon in the plerixafor group was slightly higher compared with the CY group ($7964 vs $7536; P=0.16).
Conclusions: Our data indicate robust stem cell mobilization in MM patients with either fractionated high-dose CY and G-CSF or G-CSF alone with preemptive plerixafor. The chemo-mobilization approach was associated with two-fold stem cell yield, slightly lower cost (including cost of hospitalization) but significantly increased toxicity.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal