Abstract
Background:
Bortezomib (BTZ), a proteasome inhibitor, is a promising agent against Multiple Myeloma (MM). BTZ induced lung injury (BLI), although not appreciated during the introductory time of the medication, has now been highlighted in multiple case reports. Two primary hypotheses for the cause of pulmonary toxicity are:
A. BTZ withdrawal leads to reactivation of Nuclear Factor (NF)- κB causing inflammatory changes in the lungs, which explains the rapid improvement of BLI with steroid therapy reported in several cases.
B. BTZ not only affects NF- κB, but also various other unclear signaling pathways. Its metabolite may accumulate in lungs causing direct toxicity. It may explain cases, which don't improve with steroid therapy.
Some anecdotes claim that genetic predisposition (especially Japanese population) and history of prior Stem Cell Transplant (SCT) might be risk factors for BLI. The objective of this study is to report a case of BLI, review current literature, and determine the predictors of mortality in BLI.
Case report:
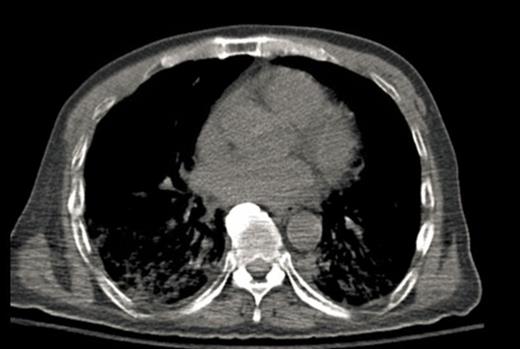
A 64-year-old male with chronic low back pain presented to the emergency department with new onset severe mid back pain radiating to bilateral shoulders. CT scan, performed to rule out aortic dissection, demonstrated multiple lytic lesions throughout the bony skeleton and a compression fracture at T7 vertebral body with epidural extension of soft tissue. A bone survey confirmed CT scan findings, and subsequent bone marrow biopsy confirmed the diagnosis of MM. He received radiation therapy to the thoracic spine and completed 2 cycles of CyBorD regimen (Cyclophosphamide 300 mg/m2 by mouth, BTZ 1.5 mg/m2 sub-cutaneous, and Dexamethasone 40 mg by mouth each on day 1, 8, 15 and 22). Three days after the completion of the second cycle, he was admitted to hospital with respiratory distress. CT chest (Image 2) showed new interval appearance of bilateral perihilar groundglass opacities, peribronchial and interstitial thickening predominantly in the upper lobes not seen in prior scan (Image 1). There were no other signs or symptoms of pneumonia such as leukocytosis, fever or cough. After some benefit from oral prednisone, he was discharged with a tapering dose of the same. Unfortunately, patient was readmitted with worsening respiratory distress 4 days later. A repeat CT scan of the chest showed resolution of previously well-defined areas of perihilar ground glass opacities but development of hazy areas of ground-glass opacification throughout both lungs with more confluent abnormalities in bilateral lower lobes (Image 3). Patient was treated with high dose methyl-prednisone and noninvasive positive pressure ventilation without any improvement. Family requested do-not-resuscitate and do-not-intubate status. Patient died on 10th day of the admission.
Methodology:
A case report, review of current literature on BLI, and analysis of available data.
Results:
An extensive Pubmed search for BLI yielded 29 cases, 5 of which occurred with re-administration of BTZ after resolution of a BLI. Mean (Standard Deviation, Minimum, Maximum) age is 60.72 years (10.12, 31, 74). 69% were males, 13.8% have smoking history, 20.7% have history of lung diseases, and 34.5% have underwent SCT for MM. 62.1% patients were on steroids concurrent with or just prior to BTZ and almost 80% were treated with high dose steroids for BLI. Mean total BTZ dose 4.62 mg (2.75, 1,9), mean duration from the 1st dose to onset of BLI 21.77 days (16.72, 0.5, 60), and mean duration from the last dose to onset of BLI was 3.27 days (2.82, 0, 10). 41.4% patients died of BLI. Mann Whitney test showed no significant difference in median age, median number of BTZ doses, and median duration from the 1st dose of BTZ to the onset of BLI between diseased and survivors. But the difference in median duration (Minimum, Maximum) from the last dose of BTZ to the onset of BLI between deceased (1.00 day, 0, 5) and survivors (4.00 days, 0, 10) were found to be statistically significant (p= 0.007). No significant association could be found between the outcome of BLI and different factors like sex, history of SCT, previous lung diseases, history of smoking, concurrent/prior steroids and treatment of BLI with steroids.
Conclusion:
BLI is a serious condition as 41.4% of the reported cases were fatal. Early onset of respiratory distress after the last dose of BTZ can be a predictor of mortality in BLI.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal