Abstract
Introduction: Lenalidomide is an immunomodulatory small molecule with efficacy in CLL, though monotherapy responses are typically partial and delayed. Plerixafor, a small molecule inhibitor of the CXCR4 receptor responsible for homing CLL to the microenvironment, has been safely utilized in CLL. The combination of plerixafor with lenalidomide offered a novel non-cytotoxic alternative to improve anti-tumor activity through targeting of the essential pro-survival microenvironment.
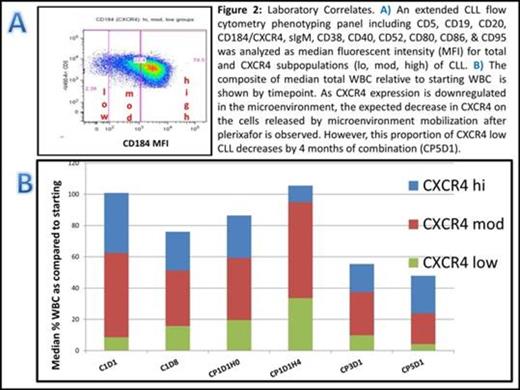
Methods: The primary objective of this single institution, open label, phase I clinical trial (NCT01373229) was to evaluate safety of daily lenalidomide in combination with escalating dose levels of plerixafor. Secondary objectives examined objective response rates, disease symptom improvement, and laboratory correlatives of the drugs’ synergy or resistance. The 3 stage study design is outlined in Figure 1. All adverse events (AEs) on combined therapy were recorded according to CTCAEv4, with dose limiting toxicity (DLT) assessment period defined as the first 28 days of combination therapy. Blood was collected throughout study conduct for analyses including an extended CLL phenotyping by flow cytometry with analysis of CLL subpopulations by CXCR4 expression levels. Phospho-protein analysis was performed by phospho-flow cytometry (phosflow).
Results: Fifteen subjects (4 female) with a median age of 62 years were enrolled, and all have completed treatment on the trial. Subjects received a median 4 (range 1-8) prior chemotherapy regimens (100% with previous alkylator and rituximab, 93% with prior fludarabine) and had poor prognostic features (73% with del 17p, 93% with unmutated IGHV). Ten subjects initiated plerixafor, and 7 completed at least 1 combination cycle. Two dose limiting toxicities (neutropenia, thrombocytopenia) occurred in plerixafor dose 2 (0.32 mg/kg), thus MTD was exceeded at this level. A total of 6 subjects completed dose cohort 1 confirming 0.24 mg/kg as the MTD. Most common grade 3/4 toxicities (>20%) on combination therapy included neutropenia (60%), thrombocytopenia (60%), and anemia (40%). Six patients reached interval response assessment and each had stable disease (SD). All response-evaluable patients derived improvement in nodal/splenic mass and disease symptoms. Of 4 subjects who completed the planned combination therapy, 2 continued on amended lenalidomide monotherapy with 1 subject obtaining a PR. Phenotyping demonstrated CD40, CD95, CD80 and CD86 significantly increased within the CXCR4 high population 4 hours post first plerixafor dose. For the five subjects completing greater than 4 months of combination treatment with end on study (EOS) samples, CD52 declined significantly; and although total WBC decreased over treatment course, the proportion of the high CXCR4 population increased with time (Figure 2). Phosflow demonstrated a significant increase of p-Erk (T202/Y204) by EOS.
Conclusions: The MTD was oral lenalidomide 10mg daily with plerixafor SQ 0.24mg/kg thrice weekly for 3 weeks of a 28 day cycle. The majority of grade 3/4 toxicities (and DLTs) were cytopenias (anemia, neutropenia, thrombocytopenia). These toxicities may have been augmented from the combination treatment, or may be a reflection of study subjects with preexisting disease or therapy related marrow suppression. Other emerging lenalidomide clinical results suggest that lower doses may produce less myelosuppression while maintaining or improving clinical benefits by decreasing treatment disruptions that precipitate disease symptoms or tumor flare. Overall, the SD and single PR among heavily pretreated subjects with very high risk features are encouraging given the duration these subjects remained on trial without progression.
Correlates demonstrated a decrease in CD52, a marker that has been previously associated to poorer CLL outcomes, and suggests a possible therapeutic effect given these subjects did not have disease progression while on treatment. Increases of CD40, CD95, CD80 and CD86 on lenalidomide monotherapy within 4 hours of plerixafor addition suggest immunomodulatory actions in circulating CLL cells (CXCR4 high expressing). Increased p-Erk by the end of trial may be an emerging resistance marker, and exploration of this effect in select patients could translate into other combination strategies that target this mechanism.
Brander:Celgene: Mentor received research funding Other. Off Label Use: This is a phase I clinical investigational study of lenalidomide and plerixafor combination in previously treated CLL/SLL.. Rizzieri:Celgene: Consultancy, Speakers Bureau; Sanofi: Consultancy. Lanasa:MedImmune, LLC: Employment; Genentech/Roche: Consultancy; Celgene: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal