Abstract
The revised international prognostic scoring system (IPSS-R) improved cytogenetic prognostic classification in comparison with IPSS classification in patients with myelodysplastic syndromes (Greenberg P et al. Blood 2012, Schanz J et al. JCO 2011). Monosomal karyotype (MK) defined as the presence of at least two autosomal monosomies or one monosomy associated with structural abnormalities has been investigated in MDS patients with contradictory results regarding its independent prognostic significance (Patnaik M et al. Leukemia 2011, Gangat N et al. AJH 2013, Valcarcel D et al. JCO 2013).
The aim of this study was to investigate the prognostic significance of MK in relation to IPSS-R and the presence of complex karyotype (CK).
The study was conducted in 391 patients with primary MDS treated at three hematology departments in Serbia. The median age was 65 years, from 15 to 89 years. There was a predominance of male patients who made 60% (235) of patients. 229 (58 %) patients died. 87 patients (22 %) transformed to AML. The sixty eight % of patients were transfusion dependent. Disease modifying treatment was applied in 48 (12.3%) of patients (AML like chemotherapy in 37 patients, low dose ara-c in 11 patients, stem cell transplantation in five patients, and in one patient azacitidine). The rest of the patients received supportive treatment.
Karyotypes were classified according to the International System for Cytogenetic Nomenclature Criteria. The inclusion of patients was based on criteria used in IPSS-R classification (a white blood cell count ≤12x109/l, an absolute neutrophil count ≤8x109/l, peripheral blood blasts ≤19%, and bone marrow blasts ≤30%).
The distribution of patients according to FAB classification was as follows: 129 (32.99%) RA, 47 (12.02%) RARS, 143 (36.57%) RAEB, 48 (12.27%) RAEB-T, and 22 (5.6%) non proliferative CMML. The classification according to WHO 2008 classification was as follows: RCUD 29 (7.43%), RARS 39 (9.97%), RCMD 90 (23.01%), RAEB1 78 (19.95%), RAEB2 65 (16.62%), AML/RAEB-T 48 (5.27%), 5q- 11 (2.81%), MDS-u 7 (1.8%), CMML 1 15 (3.83%), CMML 2 7 (1.8%).
IPSS-R distribution was: very low risk 38 (9.71%), low risk 108 (27.6%), intermediate risk 86 (21.99%), high risk 83 (21.23%), very high risk 74 (18.9%). Two patients could not be classified because of lack of all data.
Median number of metaphases was 15, from 2 to 30. The abnormal karyotype was found in 166 (42.45%) patients.
CK defined as the presence of at least three cytogenetic aberrancies was present in 32 patients (8.18%) with median survival of 5 months. CK shown prognostic significance regarding the overall survival (OS) (p = 0.00001) as well as time to AML transformation (p = 0.00014).
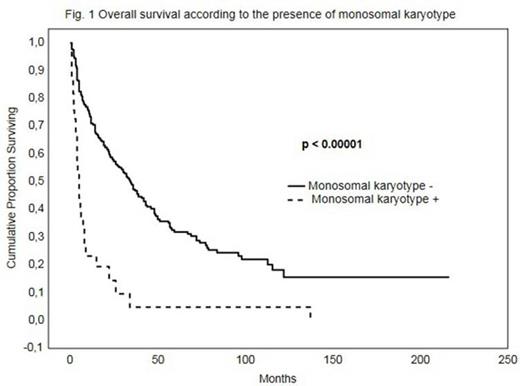
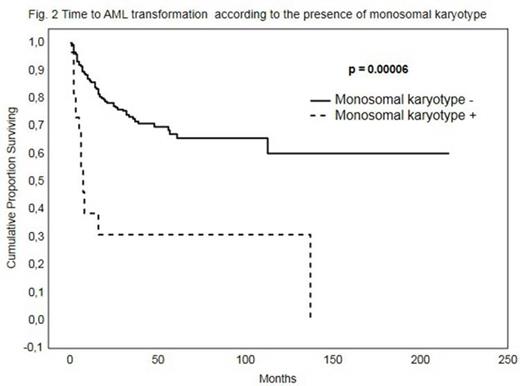
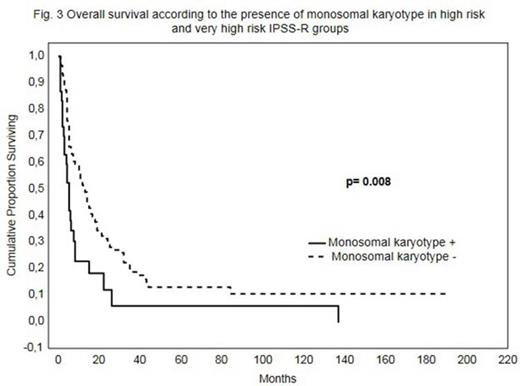
MK was detected in 34 patients (8.69%). The patients with MK had significantly shorter OS in comparison with patients without MK (median survival 5 months versus 34 months, p < 0.00001, Figure 1) as well as a shorter time to AML transformation (p = 0.00006, Figure 2). If we included only the patients who have MDS according to 2008 WHO classification MK shown prognostic significance for OS (p = 0.00121) as well as for time to AML progression (p = 0.00010). The presence of MK defines the group of patients with shorter OS in high risk and very high risk IPSS-R prognostic groups (p=0.008, Figure 3). In multivariate analysis, MK shown to be independent predictor of poor survival together with age, haemoglobin concentration, platelet count and bone marrow blast cells (p<0.001, HR 2.97, 95% CI 1.91-4,66) as well as for the risk of AML transformation with bone marrow blasts and platelet count (p<0.001, HR 3.44, 95% CI 1.79-6.61).
In 29 patients MK was associated with CK. However, in five patients (16% of MK + patients) with monosomy and an additional aberration who do not fulfil the criteria for CK the OS seems to be very short (median survival 3.5 months). The significance in OS between this small group of patients and other patients excluding the patients with CK was not significant (p=0.09). Yet, only in one case of MK cytogenetic aberrations were defined as high risk according to IPPS-R cytogenetic classification.
In conclusion, MK has an independent prognostic significance for survival and risk of AML transformation in MDS patients particularly in high and very high risk IPSS-groups. In majority of patients with MK there is an association with complex karyotype. Yet, there are a few patients with MK who do not have CK and seems to have unfavourable prognosis.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal