Abstract

Background: The natural history of sickle cell disease (SCD) includes premature death. Advancements in care, such as penicillin prophylaxis, have made death during childhood uncommon. Prior survival estimates for adults with SCD have been limited by survival bias (subjects enrolled as adults) or the limitations of administrative data. No prior study has estimated survival for adults with SCD from a newborn cohort. Herein, we report an continued observation of subjects in the Dallas Newborn Cohort (DNC)1.
Methods: The DNC is an inception cohort of patients with SCD defined by: (1) diagnosis by Texas newborn screening after October 31, 1983; (2) evaluation in the pediatric sickle cell program at UT Southwestern (UTSW) / Children’s Medical Center Dallas (CMCD); and (3) confirmation of SS, SC, Sβ0 or Sβ+ genotype. Patients followed at CMCD are transitioned to adult care before the 19th birthday. To identify transitioned patients or those lost to follow-up (LTFU), we reviewed the medical records at Parkland Memorial Hospital (PMH) and UTSW University Hospital (UH), the public and private hospitals affiliated with CMCD and the most common care-sites for transitioned patients. In addition, for patients no longer actively followed at CMCD, we queried the National Death Index (NDI). The NDI is a centralized database of death records obtained from all state vital statistic bureaus in the US and is maintained by the National Center for Health Statistics. As of our query in April 2014, deaths occurring from 1/1/79 - 12/31/11 were available in the NDI. Probabilistic matching is performed by the NDI to identify subjects using identifiers such as name, social security number, birthdate, gender, state of birth, and race. Patients who were LTFU or transitioned to adult care were censored at 12/31/11 or the date of their last clinical encounter, whichever occurred latest. Patients actively followed at CMCD, PMH, or UH were censored at 12/31/13.
In addition to descriptive statistics, we constructed survival curves using the Kaplan-Meier method to evaluate overall survival and survival by genotype. Also, Cox Proportional Hazard modeling was used to assess genotype, baseline hemoglobin, baseline reticulocyte count (%), and baseline oxygen saturation as potential predictors of early mortality. To test the sensitivity of the NDI to identify deceased individuals, we submitted 36 known deaths from the cohort.
Results: The DNC is now comprised of 1214 patients with 16,636 years of follow-up. The cohort is 49.2% female with a mean age, and duration of follow-up, of 13.2 years (Range 0.1 – 30.0 years). SCD genotypes included 60.5% HbSS, 30.6% HbSC, 6.8% HbSβ+, and 2.1% HbSβ0. Of the 1214 patients in the cohort, 511 were active in the pediatric program, 195 were in the pediatric age range but had moved or were LTFU, 238 were adults with 1 or more visits at PMH or UH, 234 were adults with no subsequent identifiable clinical encounters, and 36 were deceased.
Of 36 known deaths submitted to the NDI, 34 were identified by their databases (94.4% sensitivity). Of the 606 patients who were LTFU or aged out of the pediatric program, only 10 were reported to have died by the NDI. One of them was confirmed to be erroneous because the patient had clinical encounters after the NDI-reported date of death. In addition to these 9 deaths in the NDI, 8 additional patients were known to have died as of 12/31/13, bringing the total number of deaths to 53 (4.3%). Of these, 21 (39.6%) have been identified since the last cohort update in 2007.
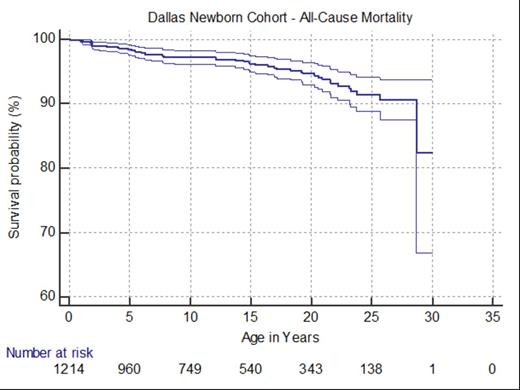
Overall survival in the DNC to age 25 years was 91.4% (95% CI: 88.4%, 93.7%) for all members (Figure), 87.7% (95% CI: 83.3%, 91%) for those with HbSS or HbSβ0, and 98.6% (95% CI: 96.7%, 99.4%) for those with HbSC or HbSβ+. In univariate analysis, early mortality was associated with SS or Sβ0 genotypes (compared to HbSC or HbSβ+), lower baseline hemoglobin, and low baseline SpO2 but not gender or reticulocytes. In multivariate analysis, early mortality was associated with only lower baseline hemoglobin (Hazard Ratio 0.76 [95% CI 0.59, 0.98], P=0.037).
Conclusions: These are the first modern estimates of survival into adulthood with an unbiased newborn cohort of SCD patients. Early mortality is associated with low baseline hemoglobin. Survival to age 20 remains excellent at 95% but the mortality rate appears to accelerate in early adulthood.
Reference: 1. Quinn et al. Blood. 115(17):3447-52, 2010.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal