Abstract
A sixty-one year-old Hispanic female with Waldenstrom’s Macroglobulinemia diagnosed in 2011 and successfully treated with 6 monthly cycles of Cyclophosphamide, Rituximab and Dexamethasone (CDR) from 12/11 through 5/12 was then put on a two-year maintenance scheme with Rituximab every three months. In February, 2014 (six months before the end of the planned treatment), she came to the ER complaining with severe headache, aphasia and blurred vision. A stroke was initially ruled out and she received Paracetamol with partial improvement. Nonetheless, symptoms re-appeared accompanied with disorientation and agitation. Antipsychotic medication was given with no improvement. On PE she was disoriented with aphasia, paraparetic and neck stiffness suggestive of meningitis. Blood tests, a MRI and lumbar puncture were performed showing leptomeningeal hyperintensity with no signs of encephalitis (Figure 1).
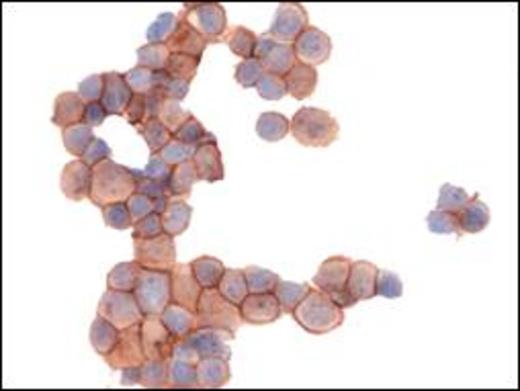
CSF analysis showed WBC 64 cells/µL, (95% MNC), glucose= 9.8 mg/dL and proteins= 110 g/dL. Gram dye was negative. A geneXpert for Tuberculosis was negative. CSF cytology showed an infiltration of lymphoid neoplastic cells confirmed by cytochemistry (Figures 2a and 2b).
With these results a Bing Neel syndrome was diagnosed and IT Methotrexate was given for a total of 6 doses resulting in a nice reduction of the neoplastic cells. However, she relapsed in April/2014 and IV Fludarabine was started. We are planning to add IT liposomal Cytarabine. Additionally, MYD 88 gene mutation was detected.
DISCUSSION: There are only 33 reported cases of Bing-Neel syndrome in the medical literature for the last 80 years and this one has been confirmed with the newest tools such as: MRI, cytochemistry and gene mutation.
CONCLUSION: Bing-Neel syndrome should be suspected in every patient with Waldenstrom’s Macroglobulinemia and CNS impairment.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal