Abstract
INTRODUCTION. Chemotherapy (CHT)-induced anemia is a consequence of the myelosuppressive effect of CHT, delivered for solid or hematologic malignancies, and tends to worsen over the course of repeated cycles of therapy. Erythropoietic agents have shown their efficacy in correcting CHT-induced anemia in cancer patients, in reducing the need of blood transfusion and in improving patients’ quality of life. Epoetin (EPO) biosimilars have emerged as an alternative to originator products, sharing an equivalent mechanism of action, efficacy and safety, as a result of a rigorously conducted comparability exercise.
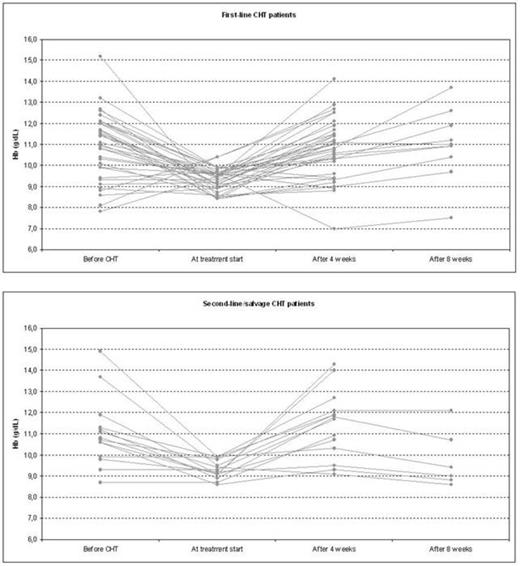
PATIENTS AND METHODS. This study was aimed at evaluating the response to EPO alpha biosimilar (Binocrit®, Sandoz, 40,000 IU/week subcutaneously) after a 4-weeks (and 8-weeks, when applicable) treatment period, as well as the rate of CHT cycles delays or interruptions due to anemia, in 49 consecutive adult patients, affected by chronic lymphoproliferative disorders, undergoing CHT, either as a first-line induction (35 patients) or second-line or salvage treatment (14 patients), and presenting with CHT-induced anemia. The median age was 69 (range 21-90) years, with 49% of the patients older than 70. Fourteen had diffuse large B-cell lymphoma, 14 an indolent non-Hodgkin’s lymphoma, 6 had chronic lymphocytic leukemia, 5 mantle cell lymphoma, 4 T-cell lymphoma, 2 hairy cell leukemia and 1 had histiocytosis. Response to EPO was defined as an increase in hemoglobin (Hb) levels after 4 (ΔHb4) and 8 weeks (ΔHb8) of treatment of at least +1 g/dL, or as the achievement of Hb > 11 g/dL independently of ΔHb, with a complete transfusion-independence. Hb stability was regarded as a ΔHb comprised between -1 and +1 g/dL. A ΔHb < -1 g/dL or an acquired transfusion dependence was judged as a lack of response. Treatment with EPO was started at the first occurrence of Hb < 10 g/dL during chemotherapy, when anemia was not due to any different concomitant cause (e.g. hemolysis, iron deficiency, malabsorption, etc). Treatment duration was established by the treating physician; however, treatment was stopped when Hb reached at least 11 g/dL, in patients whose chemotherapy programme had reached its completion and in those who became transfusion dependent.
RESULTS. Mean Hb (± standard deviation) at presentation was 11.0 ± 1.6 g/dL, with 49% of patients being anemic mostly as a consequence of their disease. Nine patients had grade 2 anemia, while one presented with grade 3 anemia. Twenty-one were treated with a cyclophosphamide, doxorubicin, vincristine and prednisone (CHOP) every 21 days or with a weekly CHOP-like regimen; 10 received a fludarabine-based regimen; 6 underwent a bendamustine-based second-line treatment. The remaining 12 patients were treated with various regimens (lenalidomide, rituximab, cladribine, temsirolimus, gemcitabine). Mean Hb level at EPO treatment start was 9.3 ± 0.5 g/dL. After 4 weeks of treatment, the reached mean Hb level was 10.8 ± 1.4 g/dL for patients receiving a first-line CHT, and 11.4 ± 1.6 g/dL for those on a second or later CHT line, with a mean ΔHb4 of 1.4 ± 1.4 g/dL and 2.1 ± 1.6 g/dL for each group of patients, respectively. Sixteen patients had their Hb level measured after 8 weeks of treatment, achieving a mean Hb level of 11.0 ± 1.7 g/dL and 9.8 ± 1.4 g/dL for each treatment subgroup, with a ΔHb8 of 1.7 ± 1.6 g/dL and 0.5 ± 1.3 g/dL, respectively. Overall, 36 patients responded to the treatment, yielding to a 73.4% hematological improvement rate. Eleven patients (22.5%) showed a stable Hb level throughout their treatment course, and 2 (4.1%) were considered non-responders (figure). Among responders, 2 patients required a new biosimilar EPO alpha treatment, again with response; 2 patients showed a late recurrence of anemia, and were managed with blood transfusions. Overall, 22 patients (44.9%; 61.1% of responders) had an Hb increase of at least 2 g/dL. CHT cycles were delayed in 9 cases (18.4%) because of anemia; interruptions of the planned CHT programme occurred in 6 cases (12.2%). No adverse events were documented; in particular, no thromboembolic or pure red-cell aplasia episodes have been demonstrated.
CONCLUSION. The treatment of CHT-induced anemia with biosimilar EPO alpha in patient with chronic lymphoproliferative disorders is correlated with a high rate of responses and allows a safe completion of the planned CHT programme in most of the cases, both in induction and salvage treatment settings.
Broccoli:Sandoz: Membership on an entity's Board of Directors or advisory committees. Zinzani:Sandoz: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal