Abstract
Tumor-infiltrating immune cells influence diffuse large B-cell lymphoma (DLBCL) outcome. Relatively little is known about the significance of peripheral blood immune cell counts (obtained by generally available flow cytometry) on DLBCL behavior
Patients and methods: 45 newly diagnosed DLBCL patients enrolled in an institutional protocol had blood pretreatment multicolor flow cytometry performed and immune cell counts recorded. The M/F ratio was 24/21, age 19-88, median 64; stage I: 11, II: 13, III: 6 and IV: 15. Thirty two had low/ intermediate International Prognostic Index (IPI) score (0-2) and 13 had 3+ IPI. One patient was HIV+. Thirty seven (82%) received immuno-chemotherapy and 8 had chemotherapy and/or irradiation.
Statistical Methods: The outcomes of the study were progression free survival (PFS) and overall survival (OS). Kaplan-Meier estimation method and Log-rank test were used in the univariate analysis. The Cox proportional hazard model was used for multivariable analysis (MVA). All analyses were done via SAS 9.2.
Results: Mean absolute CD4 cell count (ACD4C) was 450/c.mm and the median about 400. After follow up of 0.8 to 152 months (median: 73), 25 (56%) were still alive.
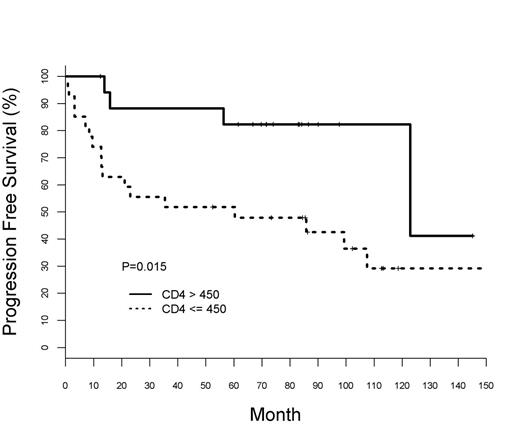
Univariate analysis: significant predictors to PFS were: age (HR=1.05, 95%CI: 1.02-1.09, p=0.005), ACD4C (HR= 0.998, 95% CI: 0.966-1.000, p= 0.023] and IPI (HR=0.05, 95%CI: 0.995-1.89, p= 0.054). But for OS ACD4C was only marginally significant (p= 0.083). Absolute lymphocyte count (ALC), CD8 and [CD3-C56+ (NK)] counts did not correlate with OS or PFS.
When analyzed as a binary variable with cutoff of 450/cmm, the 18 patients with high ACD4C had better 5 year PFS, 88% vs. 52% (p= 0. 023), figure (1), and OS, 88% vs. 59% (0.054) than the 27 with low ACD4C. Age, IPI groups (low /intermediate versus high) and ALC also correlated with PFS and OS, but not the CD8 or NK cell counts.
MVA with age as a continuous variable, IPI groups and ACD4C of 450/cmm; age and ACD4C only were significant for PFS, (p= 0.008 and 0.036 respectively). For OS age was the only significant variable (p=0.017). ALC, CD8 and NK cell counts did not correlate with PFS or OS.
Conclusion: Though the series contains more early stage patients than usual, blood ACD4C seems to be a predictor of PFS and to a lesser extent OS in DLBCL independent of age and IPI. If confirmed in a larger prospective study of uniformly treated patients ACD4C may serve as an immunological marker for DLBCL biological behavior.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal