Abstract
Background
Obesity has been pointed out as one of the risk factors for the development in several neoplastic diseases including malignant lymphoma. However the impact of obesity on the outcome of malignant diseases is unclear. L.Weiss et al have shown that high body mass index (BMI) is a significantly better prognostic factor in diffuse large B-cell lymphoma (DLBCL) (Increased body mass index is associated with improved overall survival in diffuse large B-cell lymphoma. Annals of Oncology 2014; 25: 171-176.). We evaluated this hypothesis in Japanese patients with DLBCL.
Patients and Methods
We analyzed 338 patients with newly diagnosed DLBCL who received full-dose (80% or more of the prescribed dose) R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone) between April 2003 and December 2009 across 7 institutes. Patients of all stages were treated 6 or 8 cycles of full-dose R-CHOP therapy. All the patients were classified into 2 groups: high BMI (≥25 kg/m2 ) or low BMI (<25 kg/m2).
Results
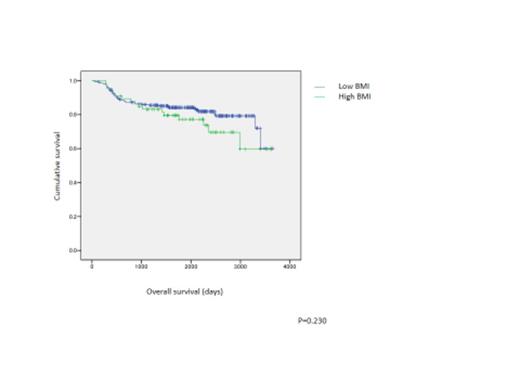
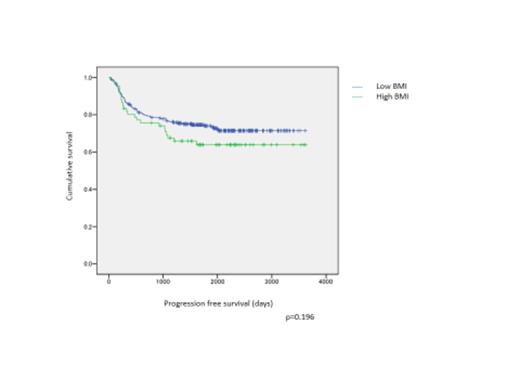
The median patient age was 65 years (19–80 years); 192 were men and 146 were women. The median BMI was 22.9 kg/m2 (14.1–40.4 kg/m2); 66 patients (19.5%) were in the high BMI group (median, 27.4 kg/m2) and 272 (80.5%) were in the low BMI group (median, 21.6 kg/m2). The median follow-up of patients who were alive (n = 271) was 67.5 months (12.6–121.8 months). The 5-year progression-free survival (PFS) and overall survival (OS) of the high versus low BMI groups were 63.9% versus 74.0% (P = 0.196) and 77.2% versus 84.2% (P = 0.230), respectively (Figure1,2). Multivariate analysis considering the sex, International Prognostic Index, B symptoms, bulky mass, and BMI showed that high BMI (≥25 kg/m2) was a significant adverse prognostic factor for both OS (hazard ratio [HR], 1.906; 95% confidence interval [CI], 1.08-3.376; P = 0.027) and PFS (HR, 1.710; 95% CI, 1.054-2.774; P = 0.030).
Conclusion
The results of our study indicated that high BMI was an adverse prognostic factor of DLBCL. It is necessary to investigate BMI and its influence on patient background or treatment in much more cases.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal