Abstract
Background
Invasive aspergillosis (IA) during induction chemotherapy of acute leukemia or allogeneic HSCT has a negative impact on the outcome of patients and is a major concern in haematology department. The impact of air treatment on invasive aspergillosis since the introduction of posaconazole prophylaxis is not very well studied at this time. In our center, the haematological intensive care unit contain ten single rooms each, of which 4 rooms are equipped with laminar airflow named “Controlled Air Zone” (CAZ) and 6 rooms have no specific air treatment (NSAT).
Objective
Our objective in this study was to compare the development of IA during hospitalization in the two areas of the unit and to analyze the impact of posaconazole prophylaxis on the short- and long-term survival. We compared the outcome of 56 consecutive patients hospitalized for induction treatment of ALL, AML or underwent allogeneic HSCT for AML/ALL in CR1 or had been hospitalized for GvHD treatment between the years 2009 and 2013. Posaconazole prophylaxis was introduced in 2013.
Results
In this study, there were 29 (52%) male and 27 (48%) female with a median age of 53 years (range, 20-64), diagnosis were AML for 35 (62.5%) patients, ALL for 11 (19.65%) patients, allogeneic HSCT for 4 (7.14%) patients (AML in CR1 for 3 and ALL in CR1 for 1), episode of aGvHD for 4 (7.14) patients and biphenotypic AL for 2 (3.57%) patients. All patients with GvHD had a grade III-IV of acute GvHD with digestive involvement. Fourty (71%) patients were hospitalized in the CAZ and 16 (29%) patients in the NSAT zone. Eleven (19%) patients received posaconazole and 45 (81%) patients received fluconazole (p=0.007).
IA was observed in 19 (34%) patients: 12 (21%) patients in the CAZ and 7 (12%) patients in the NSAT zone with a median time of 2.7 months (range, 0.3-20.50) since disease diagnosis. Twenty-five (44.6%) patients died in this study: 21(37.5%) from relapse and 4 (7%) from aspergillosis.
After a median follow-up of 12.23 months (range, 0.4-54), the probability of survival at 6 months and 12 months was for patients in CAZ: 72.5% and 64.44% respectively and for patients not in CAZ: 67.71% and 54.17% respectively. The probability of survival at 6 months and 12 months for posaconazole patients was 90% for both, and for fluconazole patients: 66.67% and 54.17% respectively. The survival according to treatment and zone is presented in Figure 1.
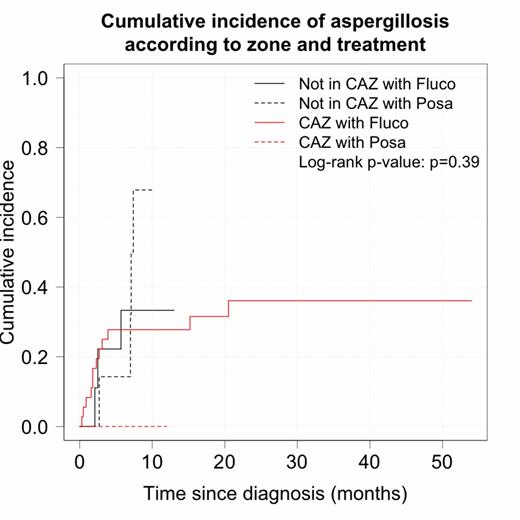
The cumulative incidence of aspergillosis at 6, 12 and 24 months for fluconazole patients: 28.89%, 28.89% and 35.88% respectively and for patients with posaconazole prophylaxis: 9.09%, 9.09% and 50%. All patients who had AI in the posaconazole group had aGvHD with digestive involvement and were hospitalized during this event in the NSAT zone. The incidence of aspergillosis according to zone was 25% and 46.88% at 6 and 12 months respectively for patients not in CAZ and for patients in CAZ: 25%, 25% and 34% at 6, 12 and 24 months respectively. For posaconazole patients in CAZ, there were no event of AI. The incidence of aspergillosis is presented according zone and treatment in Figure 2.
In univariate analysis, we found an impact of gender (p=0.045), ALL (p<0.001), GvHD (p=0.099), age (p=0.029) and a trend for CAZ (p=0.36) and posaconazole (p=0.79). The multivariate analysis shows a significant impact of age (HR= 1.06 [1.01-1.1], p = 0.019), gender (HR = 0.39 [0.14-1.09], p =0.07), ALL (HR=8.4 [2.27-31.09], p = 0.0014) and confirm a trend for CAZ (HR 0.6 [0.16-2.24], p = 0.45) and posaconazole (HR 0.66 [0.09-4.85], p = 0.6) despite non-significant p-values because the incidence curves cross in both case.
Altough this study concerning a small number of patients, IA was associated with age, male gender and ALL diagnosis. Protective factor is female gender and there is a trend for CAZ and posaconazole.
Conclusion
In conclusion, we found a trend for a protective impact of Controlled Air Zone and we confirm the impact of posaconazole prophylaxis on survival. The global environmental strategy in haematologic department associated with antifungical prophylaxis have an important impact in the management of AI and large prospective studies are needed to improve this strategy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal