Abstract
Introduction
Up to 14% of individuals with systemic AL amyloidosis develop acquired factor X (FX) deficiency, which occurs due to adsorption of FX onto amyloid fibrils. Although baseline FX level is not predictive of bleeding risk in these patients, serious hemorrhagic complications can occur, particularly during invasive procedures. Optimal management strategies to attenuate bleeding risk in these patients are unknown.
Methods
We describe our experience in the management of acquired FX deficiency, secondary to systemic AL amyloidosis, in a case series of 3 patients who received prothrombin complex concentrates (PCCs) for treatment and prevention of bleeding events. We performed a retrospective review extracting information on baseline demographics, laboratory data, pharmacokinetic (PK) studies and clinically documented bleeding events.
Results
Clinical characteristics and individual management plan are listed below:
Patient 1
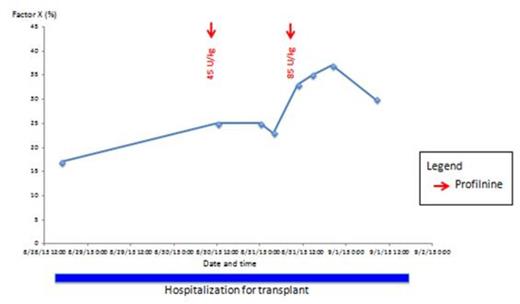
A 65-year-old man (baseline FX, 17%) was admitted for an autologous hematopoietic stem cell transplant. Given the risk of bleeding from chemotherapy-induced thrombocytopenia, the patient underwent PK studies to establish his individual dosing and frequency. On day 0, he received 45 U/kg of Profilnine. FX levels at 1- and 12-hour post-infusion are shown in Figure 1. On day +1, he received a higher dose of Profilnine at 85 U/kg. FX levels at 1, 12 and 24-hours post-infusion are shown in Figure 1. The patient had an uncomplicated hospitalization with no bleeding complications. No further PCCs were required.
Patient 2
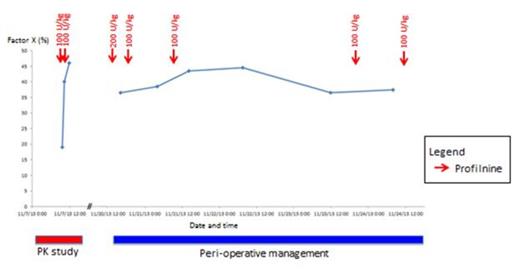
A 34-year-old woman (baseline FX, 18%) was scheduled to undergo an elective cholecystectomy. PK studies prior to her surgery and peri-operative management with Profilnine during surgery are shown in Figure 2. There were no bleeding complications. She subsequently underwent an autologous hematopoietic stem cell transplant without any replacement therapy. No complications occurred.
Patient 3
A 65 year-old woman (baseline FX, 7%) underwent a transjugular liver biopsy as part of her work-up for systemic amyloidosis. Pre-procedure, she received 100 U/kg of Profilnine with a rise in FX levels to 13% (Figure 3). A repeat dose of Profilnine at 200 U/kg further increased her levels to 30%. There were no immediate complications from the procedure. The following day, she was started on induction chemotherapy with cyclophosphamide, bortezomib and dexamethasone for treatment of systemic amyloidosis. 7-days post-liver biopsy, she became hypotensive despite aggressive fluid resuscitation. A computed tomography (CT) of her abdomen revealed a large right hepatic lobe hepatoma and large volume hemoperitoneum, with at least one intrahepatic focus of active extravasation. Acute management of her bleeding event with multiple PCCs is shown in Figure 3. She also underwent embolization of her right hepatic artery. After 5 days, the patient stabilized hemodynamically, no longer requiring any factor replacement therapy. The patient opted to be discharge home on hospice care.
Conclusion
This case series demonstrate that individuals with acquired factor X deficiency secondary to amyloidosis respond variably to PCCs. This is likely due to the fact that these individuals have distinct amyloid load and fibril sequence resulting in different binding avidity for FX. This highlights the importance of performing PK testing prior to any invasive procedures to determine the dose and frequency interval to achieve adequate FX levels for hemostasis, given the variable response between individuals.
Off Label Use: Profilnine, Bebulin and KCentra are being used to replete Factor X.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal