Abstract
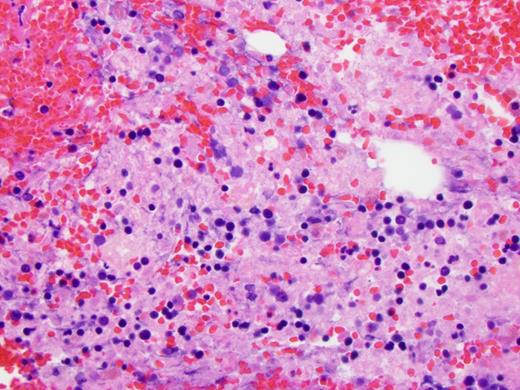
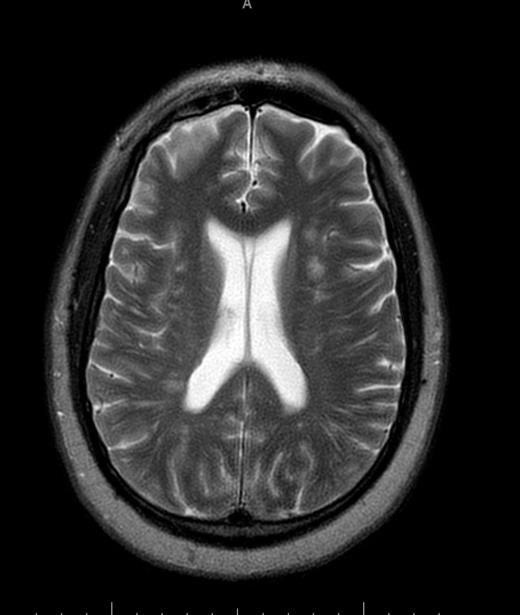
The variant sickle cell hemoglobinopathies have a variety of phenotypic presentations. Sickle cell beta plus thalassemia is an uncommon variant with an incidence that is 1/10th of sickle cell trait. This phenotype usually is associated with a milder clinical course, however often the first clinical presentation of such patients can be fatal vaso-occlusive crisis. Our case involves a 47 year old African American male with a reported history of sickle cell trait presenting with acute on chronic lower back pain for which an organic cause could not be identified with plain Xrays. He was treated with benzodiazepines and narcotics and later admitted to the ICU after being found unresponsive at home. He required intubation for airway protection. He was started on a Narcan drip for presumed narcotic overdose, without improvement. Noncontrast CT imaging of the head was negative. Laboratory findings were significant for anemia, thrombocytopenia, leukocytosis, acute kidney injury and elevated liver enzymes. Hemolysis was suspected with a markedly elevated LDH. Peripheral smear showed mild microangiopathic changes with 0-1 schisctocytes per hpf without evidence of sickle cells. Hematology was consulted and the patient was started on plasma exchange for a presumed diagnosis of TTP, however it was discontinued when his ADAMTS13 returned at a low-normal 67%, and TTP was felt less likely. MRI of the brain showed multiple focal and patchy areas infarcts throughout white matter of both cerebral hemispheres. MRI of the lumbar and thoracic spine showed a heterogeneous appearance of the bone marrow, concerning for a marrow infiltrative process. Work up for infectious or vasculitic causes were unremarkable. Hemoglobin electrophoresis showed Hb A1 20.2 (L), A2 5.8 (H), Hb F 2.2 (H), Hb S 71.8 (H), identifying doubly heterozygous sickle cell beta plus thalassemia. Bone marrow biopsy was hyperplastic with areas of geographic necrosis with sickle cells causing sludging and congested sinusoidal spaces suggesting ischemic necrosis due to vaso-occlusion. He was treated with exchange transfusion, with repeat hemoglobin electrophoresis showing A1 73.2 (L), A2 3.5 (H), HbS 23.3 (H). His lupus anticoagulant was positive raising concern for APLAS contributing to his catastrophic clinical course and severe neurologic disease,so he was started on anticoagulation with Lovenox and high dose steroids at a dose of 1 mg/kg daily. When the anticardiolipin and beta2 glycoprotein antibodies returned negative, the steroids were tapered and eventually discontinued. The clinical significance of the lupus inhibitor remains unclear. Shortly after initiation of plasma exchange and simple transfusion, the patient did stabilize hematologically. Platelets returned to the normal range and there was no evidence to suggest ongoing hemolysis. Renal and liver function improved. However he made no neurological recovery. He continued to require ventilator support and underwent a tracheostomy. A repeat MRI head showed progressive infarcts of both cerebral hemispheres, with new cerebellar infarcts. He was declared brain dead after 23 days and care was withdrawn. This case demonstrates that sickle cell beta plus thalassemia can present with acute hemolysis and bone marrow necrosis in otherwise healthy adults. The literature supports bone marrow necrosis and subsequent fat emboli as the likely pathophysiologic nidus responsible for multiorgan system failure including the catastrophic neurologic insult in this patient. Prompt recognition of this uncommon and challenging disease presentation and timely treatment with exchange transfusion may lead to improved clinical outcomes.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal