Abstract
Background : Patients diagnosed with myeloproliferative neoplasms (MPNs), including myelofibrosis (MF), polycythemia vera (PV), and essential thrombocythemia (ET), experience disease burdens that can negatively affect their quality of life. Disconnects between patient and physician perceptions of disease burden or poor patient-physician communication may delay or prevent achievement of treatment goals. The MPN LANDMARK SURVEY is the first large US-based survey designed to evaluate disease burden and patient-physician communication in MPN disease settings.
Methods : All eligible patients diagnosed with 1 of the 3 MPNs and physicians treating patients with MPNs that were recruited were surveyed in the US during May-July 2014.The surveys included ≤67 questions (depending on the type of MPN and respondent) and required approximately 20–25 minutes to complete. Descriptive analyses were conducted to identify gaps in perceptions of disease burden and patient-physician communication.
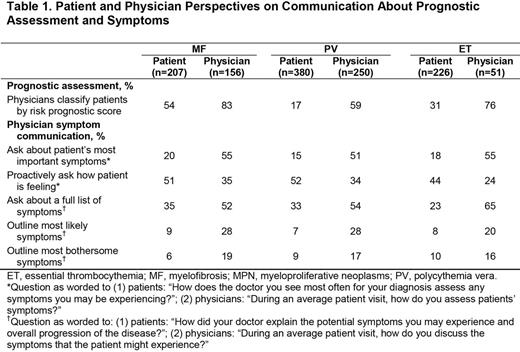
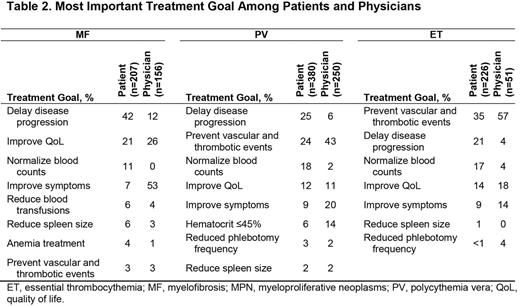
Results : The MPN LANDMARK SURVEY was completed by 813 patients (MF=207; PV=380; ET=226) and 457 physicians. Approximately half of the patients were 60–74 years of age (MF, 55%; PV, 51%; ET, 46%), the majority were female (MF, 54%; PV, 62%; ET, 72%) and had a degree from a 4-year college or postgraduate institution (MF, 65%; PV, 65%; ET, 58%), and >98% had health insurance. The majority of physicians graduated from medical school 5–24 years before the survey (67%) and practiced in outpatient settings (single specialty groups, 42%; academic hospitals, 31%). Patient-physician communication gaps were identified in several important areas: (1) Prognostic assessment: most patients did not recall receiving a prognostic risk score, but most physicians reported classifying patients by prognostic risk (Table 1). (2) Symptom assessment: physicians were more likely than patients to report that physicians ask about patients' most important disease-related symptoms or about a full and comprehensive list of symptoms (Table 1). (3) Treatment goals: the most important treatment goals were different in MF (patients: delay disease progression; physicians: improve symptoms) and PV (patients: delay disease progression; physicians: prevent vascular/thrombotic events) settings (Table 2). Patients and physicians in the ET setting both reported that prevention of vascular/thrombotic events was the most important treatment goal. Patients and physicians in the MF and PV settings reported fatigue as the most pressing disease manifestation that patients would like to resolve (MF: patients, 47%; physicians, 65%; PV: patients, 33%; physicians, 31%), whereas patients and physicians differed in the ET setting (patients: fatigue, 33%; physicians: stroke, 29%). Most patients reported a desire to be ≥50% responsible for their treatment decisions (MF, 72%; PV, 71%; ET, 75%). Physicians reported that most patients sometimes or often did not wish to comply with their primary treatment recommendation (MF, 77%; PV, 84%; ET, 79%). (4) Treatment satisfaction: overall, more than one third of patients were somewhat satisfied or dissatisfied with their physician's communication about their condition and treatment (MF, 34%; PV, 43%; ET, 45%) and with their physician's overall management of their disease (MF, 36%; PV, 40%; ET, 42%). Among patients who changed their MPN doctor (MF, 47%; PV, 46%; ET, 56%), dissatisfaction with prior care received was the most frequently reported reason for the change (MF, 40%; PV, 37%; ET, 33%). Approximately one fifth to one fourth of patients included their doctor's office among the most helpful sources of information about their diagnosis (MF, 27%; PV, 22%; ET, 20%), and most patients included the internet among the most helpful sources (MF, 90%; PV, 87%; ET, 89%).
Conclusion : Important disconnects exist between patients' and physicians' perceptions in MPN disease settings. In addition, the majority of physicians report classifying patients by prognostic risk, including PV and ET settings, which do not have widely accepted prognostic risk scores. Although physicians generally appreciate the burden that MPNs have on patients, patient management may be enhanced with improved elucidation of patient symptoms and clear communication regarding the goals and potential benefits of interventions.
Mesa:Incyte Corporation: Research Funding; CTI: Research Funding; Gilead: Research Funding; Genentech: Research Funding; Eli Lilly: Research Funding; Promedior: Research Funding; NS Pharma: Research Funding; Sanofi: Research Funding; Celgene: Research Funding. Miller:Incyte Corporation: Honoraria, Research Funding. Thyne:Incyte Corporation: Speakers Bureau. Mangan:Incyte Corporation: Membership on an entity's Board of Directors or advisory committees; Alexion Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees. Goldberger:Incyte Corporation: Membership on an entity's Board of Directors or advisory committees. Fazal:Incyte Corporation: Consultancy, Research Funding, Speakers Bureau; Gilead: Research Funding, Speakers Bureau. Ma:Incyte Corporation: Consultancy. Wilson:Incyte Corporation: Honoraria. Dubinski:Incyte Corporation: Employment, Equity Ownership. Boyle:ICF International: Employment, Equity Ownership. Mascarenhas:Novartis Pharmaceuticals: Research Funding; Incyte Corporation: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal