Abstract
Background: Anemia is a common complication of cancer and its treatment, causing fatigue, drowsiness, depression, dyspnoea, tachycardia, dizziness and reduced quality of life. Yet, little data exist on the burden of chemotherapy induced anemia (CIA) in current oncology practice.
Methods: Patients diagnosed with incident cancers of breast, lung, colon/rectum, stomach and ovary who received chemotherapy were identified from Kaiser Permanente Southern California Health Plan (2010-2012). Patients who had a diagnosis of myelodysplastic syndrome or anemia before chemotherapy (i.e., diagnosis of inherited anemia or hemoglobin measurement <10g/dl within 3 months of chemotherapy) were excluded. We also excluded patients who received a transfusion within 2 weeks or radiation within 4 months prior to chemotherapy initiation, or who had bone marrow transplantation within 12 months prior to chemotherapy or during chemotherapy. All clinical data were collected from the health plan’s electronic medical records. Anemia was classified as grade 1: 10 g/dL to lower limit of normal (14 g/dL for men and <12 g/dL for women) ; grade 2: 8.0-9.9 g/dL; grade 3: 6.5-7.9 g/dL; and grade 4: <6.5 g/dL. The type of anemia was determined based on mean corpuscular volume (MCV) and mean corpuscular hemoglobin (MCH). Incidence proportions of patients developing CIA and 95% confidence intervals were calculated overall and by CIA severity and type, as well as by stage at cancer diagnosis, and by chemotherapy regimen and cycle.
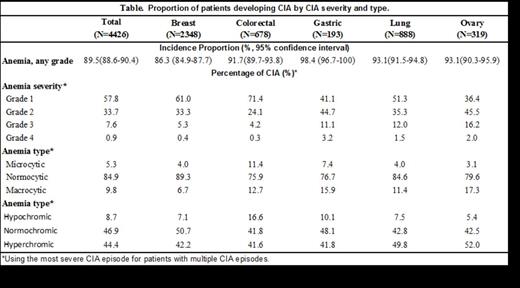
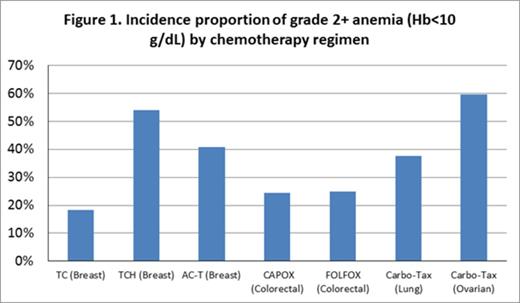
Results: A total of 4426 patients who received chemotherapy were included. The mean age was 59.3 years. Across cancers, 3962 (89.5%) patients developed anemia during the course of chemotherapy (58% grade 1, 34% grade 2, 8% grade 3 and <1% grade 4; normocytic 85%, macrocytic 10%, microcytic 5%; normochromic 47%, hyperchromic 44%, hypochromic 9%; Table 1). The incidence proportion of grade 2+ anemia ranged from 26.3% in colorectal cancer patients to 59.2% in ovarian cancer patients. The risk of grade 2+ anemia was greater in stage IV (49%), compared with 29% in stage I. The risk of severe anemia (grade 3+, Hb<8 g/dL) was highest in patients with ovarian cancer (16.9%), and lowest in patients with colorectal cancer (4%). The incidence of grade 2+ anemia during the course of chemotherapy varied from 18.2% in breast cancer patients treated with TC (CYCLOPHOSPHAMIDE|DOCETAXEL) regimen to 59.7% in patients with ovarian cancer receiving Carbo-Tax (carboplatin + paclitaxel) regimen (Figure 1).
Conclusion: Our study suggested that the burden of anemia remained high in patients with solid tumors receiving chemotherapy. The risk of anemia is greater in patients with distant metastasis. The incidence of anemia varied significantly by chemotherapy regimens.
Xu:Amgen: Employment, Equity Ownership. Xu:Amgen Inc.: Research Funding. Page:Amgen Inc.: Employment, Equity Ownership. Sattayapiwat:Amgen Inc.: Research Funding. Rodriguez:Amgen Inc.: Research Funding. Chao:Amgen Inc.: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal