Abstract
Introduction:
Asymptomatic or smoldering multiple myeloma (SMM) is usually 10-15% of all patients with multiple myeloma. Currently, national guidelines do not recommend early treatment of SMM though the majority of patients progress to active disease over time. Multiple trials have been conducted to evaluate implications of early therapy for SMM. Some of these trials, most notably, Mateos et al. (N Engl J Med 2013; 369:438-447) have shown benefit for treating SMM. However, there is lack of consensus as to whether early treatment of SMM prior to symptomatic disease progression is superior to observation alone. Hence we conducted a meta- analysis to determine if observation or treatment is superior in the management of SMM.
Methods:
We searched MEDLINE, the Cochrane database and hand-search of articles to identify 12 clinical trials which allocated SMM patients to treatment. Study quality was assessed using the Cochrane risk of Bias tool. Our main outcomes were progression free survival (PFS) and overall survival (OS). Sub-analysis examined the difference in treatment with antineoplastic agent (C), bisphosphonates (B), or their combination (CB). Data were pooled using a random effects meta-analysis using STATA (College Station Texas, V13.2).
Results:
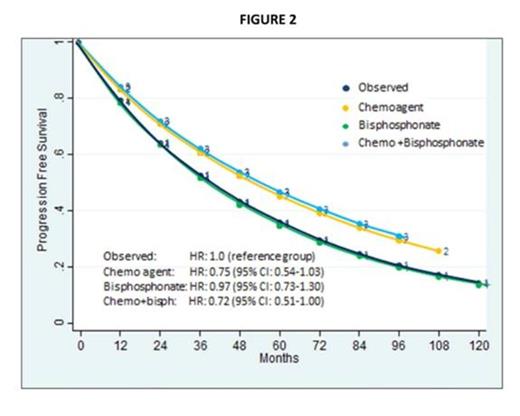
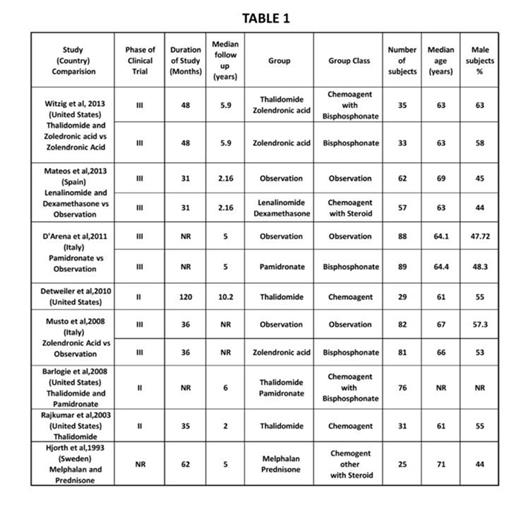
Among the 12 trials, 4 trials were excluded due lack of survival curves for OS, PFS, TTP. Characteristics of the 8 included clinical trials are given in Table 1. Participants treated for early SMM had reduced mortality (HR: 0.64, 95% CI 0.4-1.0) and better PFS (HR=0.83, 95% CI, 0.64-1.07) compared to the observation group. In subgroup analysis, patients treated with either antineoplastic agents or the combination of antineoplastic agents and bisphosphonate had a better OS and PFS, whereas therapy with only bisphosphonate did not impact OS or PFS (Figures 1, 2).
Conclusion:
We conclude that antineoplastic treatment or a combination of antineoplastic agents and bisphosphonates is better than observation in improving overall survival in SMM patients. A similar trend is seen with PFS. This conclusion merits caution given the limited data available and the differences in the agents used for therapy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal