Abstract
Introduction: AL amyloidosis (AL) and Light Chain Deposition Disease (LCDD) are plasma cell dyscrasias in which misfolded monoclonal light chains form insoluble extracellular protein deposits (fibrillar and amorphous, respectively). In AL particularly, toxic soluble light chain oligomers also play a role in disease pathogenesis. Treatment of AL and LCDD aims at eliminating the abnormal plasma cell clone. Typical agents used include corticosteroids, bortezomib (btz), alkylators, or immunomodulatory drugs (IMiDs) such as lenalidomide (len) or pomalidomide (pom). Len-btz-dexamethasone (dex) is a highly efficacious frontline regimen commonly used for multiple myeloma, a related plasma cell cancer. Despite this, prospective studies using btz-IMiD combos as initial therapy of AL or LCDD are lacking. Here we report our experience with pom-btz-dex(PVD) for pts with AL or LCDD.
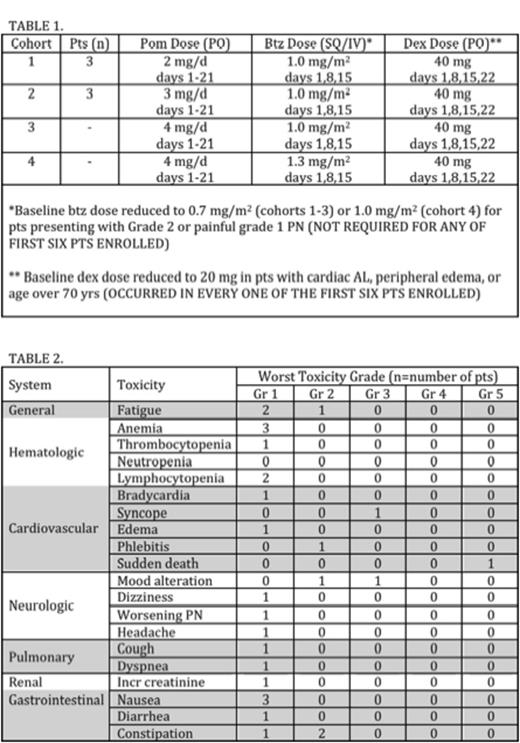
Methods: This is a prospective Phase I trial using a standard 3+3 dose escalation scheme (described in Table 1). The primary objective is to establish the maximally tolerated dosing (MTD), with assessment for dose limiting toxicity (DLT) extending through cycles 1 and 2 for each pt. Hematologic and organ responses (HR and OR) were assessed using recently updated guidelines. PVD was administered in repeating 28-day cycles until either DLT or progressive disease. Key inclusion/exclusion criteria: biopsy proven AL amyloidosis or LCDD; no more than 1 prior cycle of anti-plasma cell therapy; measurable disease defined as at least a 5 mg/dL difference between the involved (iFLC) and uninvolved (uFLC) serum free light chains, or a serum M-protein of 0.5 g/dL or greater (latter not permissible without measurable sFLCdifference after protocol amendment); ECOG PS of 2 or less; adequate renal, hepatic, and marrow function; no Grade 3 or higher peripheral neuropathy (PN; pts with painful grade 2 PN also excluded). Abnormal left ventricular ejection fraction or cardiac biomarkers allowed, but pts with NYHA class III/IV congestive heart failure or uncontrolled ventricular arrhythmias were excluded. Antithrombotic/antiviral prophylaxis was required for all pts.
Results: Six pts have been enrolled thus far (3 each in cohorts 1 and 2, respectively). Three additional pts have already been identified for cohort 3. Five of 6 pts had AL, and 1 had LCDD. Median age was 65.5 yrs (range 49-74 yrs). 5 pts were female. Mayo cardiac stage I/II/III in 1, 2, and 3 pts, respectively. Three pts had one prior cycle of therapy (the others had none). The iFLC was lambda type in all 5 AL pts, and kappa for the pt with LCDD. Median number of organs involved by AL/LCDD was 2 (range, 2-4; 4 with both cardiac and renal, and 1 additional pt with cardiac). The median number of PVD cycles administered was 3 (range 1-6). Two pts are still on therapy. The reasons for stopping PVD in the other 4 pts were: sudden death due to underlying cardiac AL (during cycle 3 of PVD), pt preference after reaching maximal HR (after cycle 6), lack of HR (after cycle 3), and toxicity (after cycle 4). Baseline dex dose adjustment was required for protocol-specified reasons in all pts. One pt required further dex reduction during cycle 4 of PVD. No pts required baseline or subsequent modification of pom or btz. Table 2 summarizes reported adverse events (AEs). No DLTshave been observed. Two pts achieved HR (0 CR, 1 VGPR, 1 PR, 3 SD, 0 PD). Organ responses have not been observed, but the first protocol-specified OR assessment takes place after 4 cycles of PVD and some pts have yet to reach this time point.
Conclusions: PVD was well tolerated in this group of pts with AL and LCDD. Importantly, no significant myelosuppression or PN was noted in the first 2 (out of a planned 4) dose cohorts. Most AEs have been related to the ptsÕ underlying AL/LCDD, though dex has posed difficulties for some pts. Hematologic responses have been seen, but organ responses are predictably lagging. Once the MTD is established, an 18-pt expansion cohort dosed at that level willfurther examine the efficacy of PVD as up-front treatment for AL and LCDD.
Zonder:Celgene: Consultancy, Research Funding; Bristol-Myers Squibb: Consultancy. Off Label Use: Pomalidomide and Bortezomib are approved drugs for multiple myeloma; they are used in this trial as treatment for the related plasma cell dyscrasias AL amyloidosis and light chain deposition disease. . Tuchman:Celgene: Honoraria, Research Funding, Speakers Bureau; Millennium: Honoraria, Research Funding, Speakers Bureau. Kukreti:Celgene: Honoraria. Burt:Celgene: Speakers Bureau. Matous:Takeda Pharmaceuticals International Co.: Speakers Bureau; Onyx: Speakers Bureau; Celgene: Consultancy, Speakers Bureau; Seattle Genetics, Inc.: Research Funding, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal