Abstract
Background
Lenalidomide (LEN) results in hematopoietic improvement in the majority of treated patients with myelodysplastic syndrome and isolated deletion of the long arm of chromosome 5 (MDS-del5q). The drug is believed to exert antiangiogenetic, antiproliferative, proerythropoietic and immunomodulatory effects. The precise nature especially of the latter mode of action is incompletely understood. While some reports in multiple myeloma argue for an immunosuppressive effect, others proposed immunostimulatory properties. This prompted us to study the effects of LEN on the adaptive immune system in a cohort of patients with MDS-del5q.
Patients, Material and Methods
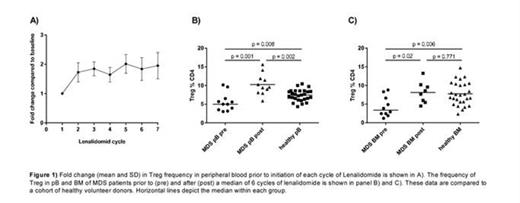
The composition of the T-cell compartment in peripheral blood (pB) and bone marrow (BM) of 11 patients with MDS-del5q treated within a multicenter, single-arm, phase II study of the German MDS study group (LEMON-5 trial) was studied by flow cytometry. Patients received LEN 10 mg per day for 21 days of each 28 day cycle. The median age was 71 years and 9 patients were female. Regulatory T-cells (Treg) were defined as CD3+CD4+CD25++CD127dimFoxP3+ while Th17 cells had to be CD3+CD4+ with positive intracellular staining for IL17 and negative intracellular staining for IFNgamma. Peripheral blood samples were taken prior to initiation of each new LEN cycle and BM specimens were obtained prior to treatment initiation and after 5 to 7 cycles of LEN. The results obtained in MDS patients were compared to a cohort of 27 healthy volunteer donors.
Results
After a median of 6 cycles all but one patient had responded with a hematologic improvement of erythrocytes, while 6 individuals achieved a complete morphologic and 5 a complete cytogenetic remission.
In comparison to healthy donors, MDS patients had significantly lower frequencies of Treg in pB (5.0 vs. 7.4 %, p = 0.008) and BM (3.4 vs. 7.4 %, p = 0.006). After initiation of LEN treatment we observed a rapid increase in Treg frequencies in pB (Figure 1A) and after a median of 6 cycles the Treg were significantly more abundant in pB (9.6 % p = 0.001, Figure 1B) and BM (8.1 %, p = 0.016, Figure 1C) compared to baseline. The median Treg frequency reached the level observed in normal donors in BM and surpassed it in pB (Figure 1B+C). Fluorescence-in-situ hybridization demonstrated that the expanded Treg were not part of the malignant clone.
Interestingly, although the median absolute lymphocyte count increased during LEN treatment (pre: 1.10 Gpt/l vs. post: 1.43 Gpt/l p = 0.013) there were no significant changes with respect to relative lymphocyte frequency (pre: 68.3 %, post: 75.61 %, p=0.499) or the percentage of T-effector cells (pre: 48.0 %, post: 51.5 %, p=0.520). Moreover, the expansion of Treg was not accompanied by a counter-regulatory increase of pro-inflammatory Th17-cells (pre: 2.3 % vs. post: 1.33 %, p = 0.328).
To address a possible mechanism of the observed Treg expansion we analyzed the concentration of transforming growth factor beta (TGFbeta), a key factor contributing to the development of Treg, in pB and BM plasma. However, LEN treatment was not associated with an increase of TGFbeta levels in these two compartments. On the contrary, the TGFbeta levels after 6 cycles of LEN were significantly lower than pre-treatment values in pB and BM (pB 4.9 vs. 2.3 ng/ml, p = 0.039; BM 4.5 vs. 0.8 ng/ml, p = 0.023).
Discussion
Our results show that LEN treatment corrects an MDS-del5q-inherent Treg deficit. This Treg expansion is not accompanied by a counter-regulatory increase in pro-inflammatory Th17 or other T-effector cells and therefore possibly results in an immunosuppressive milieu, which might contribute to the beneficial effects of the drug on myelodysplastic hematopoiesis but may also facilitate leukemic progression.
Platzbecker:Celgene: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal