Abstract
BACKGROUND: Allogeneic hematopietic cell transplantation (HCT) is still an important option of treatment in CML patients failing respond to tyrosine kinase inhibitors (TKIs). The revised European LeukemiaNet 2013 suggests HCT to be reserved for the patients in chronic phase (CP) unless resistant or intolerant to at least one second-generation TKI. The present retrospective study attempted to evaluate transplant outcomes in 85 CML patients with TKI failure, and to compare their long-term outcomes with TKI naïve or high risk CML patients responsive to TKIs transplanted in the contemporary period between 2002 and 2014.
METHODS: A total of 85 patients with TKI failure CML were transplanted in 3 transplant centers in Canada (Toronto, Hamilton and Ottawa) performed between 2002 and 2014. We reviewed the transplant outcomes of CML patients with TKI-resistance (n=74) or intolerance (n=11) with poor (n=7) or good response to TKI (n=4). TKI resistance group (group A) includes CP1 (n=26), CP2/3 (n=29) or accelerated [AP]/ blastic crisis [BC] (n=19) at HCT, while TKI intolerant group (group B) includes CP1 (n=9) or CP2/3 (n=2) at HCT. In 12 patients (14.1%), ABL domain mutations were noted as follow in 11 patients including T315I (n=6). Emergence of additional cytogenetic abnormalities (ACAs) in Ph+ clones prior to HCT was noted in 21 patients while 6 patients showed clonal evolution (CE) in Ph(-) clone. Seventy five patients (88%) received myeloablative conditioning, with 48 (57%) from unrelated donor.
As a control, 33 CML patients transplanted between 2002 and 2012 but without TKI failure were included for comparison. They were TKI naïve CP (n=22) or high risk (i.e. AP or BC) with good response to TKI (n=11). Overall survival (OS), non-relapse mortality (NRM) and relapse incidence were analyzed. Outcomes of post-transplant TKI therapy were also evaluated for planned TKI (n=3) or for treatment of relapsed CML (n=16). Serial BCR-ABL transcript levels in the first 12 months were analyzed for Receiver operating characteristic (ROC) analysis.
RESULTS: With a median follow-up duration of 113 months among survivors in patients with TKI failure, the 3-year OS rate and relapse incidence was 45±6% and 35±3%, respectively. NRM was 40±7% at 3 year. Fifty nine patients (69%) responded to HSCT: 43 (51%) achieved MR4.5 within first 12 months post-transplant. Median time to achieve major molecular response (MMR) and MR4.5 after HCT was 4 months and 10 months. Post-transplant TKI therapy was given in 16 patients as planned (n=2) or for treatment of relapse (n=14; hematologic, n=10; cytogenetic, n=1; molecular relapse, n=3). Out of 16 patients, 5 patients relapsed within median of 39 months. There was no difference in progression between the groups with hematologic vs cytogenetic/molecular relapse (p=0.39).
Transplant outcomes were compared according to the disease stage at HCT. Significant differences were noted within TKI failure group with OS rate at 3 years being 66%, 32% and 24% for those in in CP1, CP2/3 and AP/BC. The 3 year OS was significantly worse in the group with ABL domain mutation (22%) than those without mutation (50%) in TKI failure group (p=0.01). However, no difference of OS was observed according to the presence of ACAs (p=0.60) or CE in Ph(-) clones (p=0.26).
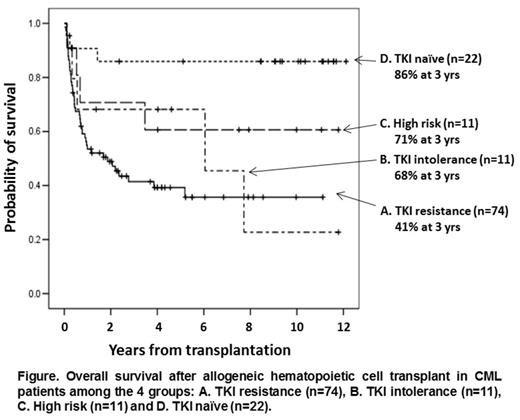
With a total of 118 patients, transplant outcomes were also compared among the 4 groups (i.e. A. TKI resistance [n=74], B. TKI intolerance [n=11], C. high risk with good response to TKI [n=11], D. TKI naïve [n=22]). High risk group (group C) includes CP2/3 (n=10) or AP (n=1) at HCT and CP (n=3), AP (n=4) or BC (n=4) at diagnosis, while TKI naïve group (group D) includes CP1 (n=21) or CP2 (n=1) at HCT and CP (n=21) or AP (n=1) at diagnosis. The OS was significantly different in favor of group D (86%) > C (71%) = B (68%) > 41% (A) at 3 years (p=0.002; Figure). Relapse incidence at 3 year was lowest in D (11%) followed by C (23%), A (32%) and B (60%).
Serial BCR-ABL transcript monitoring in first 12 months showed rapid decline of the level in the first 3 months, then decrease gradually to 12 months. ROC analysis suggested 4.3 log reduction at 3 months as strong predictive level of MR4.5 achievement in first 12 months after HCT with AUC of 0.916 (sensitivity, 73.1% and specificity, 100%).
CONCLUSION: Allogeneic HCT remains an important treatment option in patients with TKI failure even in the era of multiple available TKIs. The 3 months BCR-ABL transcript level may guide initiation of post-HCT TKI.
Walker:Sanofi: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal