Abstract
Introduction
The watch and wait (WW) strategy has been regarded as one of the standard approaches in patients with asymptomatic follicular lymphoma (FL) regardless of their tumor burden. However, the impacts of initial WW on treatment efficacy, outcomes and histologic transformation in FL patients in the rituximab era remain elusive.
Patients and methods
We retrospectively analyzed 348 consecutive patients who were initially diagnosed as having FL of grade 1 to 3a at our institution between 2000 and 2012. We analyzed time to treatment failure (TTF), and compared patients who underwent treatment following WW with those who immediately received treatment without WW. Both overall survival (OS) and time to transformation in the WW cohort and the immediate treatment cohort were also analyzed. In this particular study, TTF was defined as the time from diagnosis until progression after the initiation of first treatment.
Results
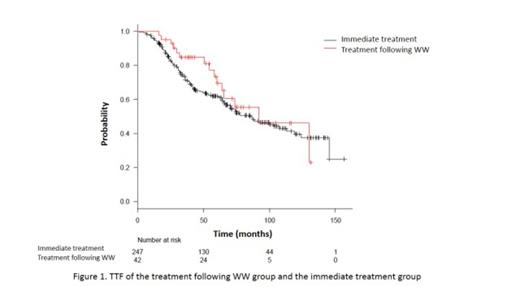
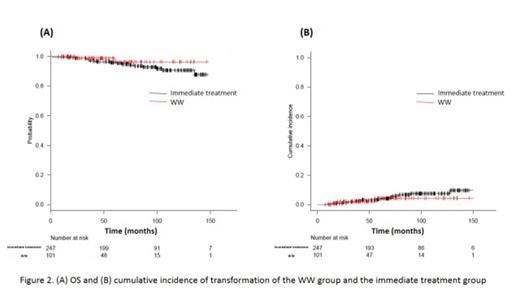
In all 348 patients with a median age of 57 years (range: 19-85), 101 patients were initially managed with WW and 247 were immediately treated at the physician's discretion. The proportions of patients with low tumor burden according to the GELF criteria were 80% (81 patients) in the WW cohort and 47% (117 patients) in the immediate treatment cohort. The median follow-up duration of all 348 patients was 75 months (range: 7-169). In the WW cohort, 45 patients (45%) received anti-lymphoma treatment, mainly because of FL progression, after a median WW duration of 16 months (range: 3-122). The majority of patients (84% in the treatment following WW group, 77% in the immediate treatment group) received a rituximab-containing regimen. The estimated median TTF in the treatment following WW cohort and the immediate treatment cohort were 92 months (95%CI, 60.1-NA) and 85 months (95%CI, 66.3-113), respectively, which were not significantly different (P=0.336) (Figure 1). In multivariate analysis, clinical stage was the predictive factor of TTF (HR 1.18, 95% CI, 1.02-1.38, P <0.05). Neither OS rate nor cumulative risk of transformation between the WW cohort and the immediate treatment cohort was statistically significant (P=0.294 and P=0.64, respectively) (Figures 2A and 2B). As risk factors of death, clinical stage (HR2.05, 95% CI, 1.12-3.75, P <0.05), age >60years (HR 3.87, 95% CI, 1.52-9.85, P <0.05) and transformation (as a time-dependent covariate) (HR 6.15, 95%CI, 1.64-23.02, P <0.05) were detected. None of the variables was significant regarding the risk of transformation. Tumor burden based on the GELF criteria was also not detected as a risk factor for treatment failure, death or transformation.
Conclusion
The results of our analysis suggested that the WW strategy does not have negative impacts on TTF, OS and histologic transformation in selected patients with FL regardless of tumor burden, indicating that this strategy can still be regarded as an acceptable approach to FL patients in the rituximab era. Further investigations, especially a prospective cohort study including evaluation of the optimal timing for starting anti-lymphoma treatment following WW, are needed to confirm our results.
Maruyama:Eisai Co., Ltd: Honoraria. Kobayashi:Behringer Ingelheim GmbH: Research Funding; Ohtsuka Pharmaceutical Co., Ltd: Research Funding; ARIAD Pharmaceutical Co., Ltd: Research Funding. Tobinai:Chugai Pharmaceutical: Research Funding; Zenyaku Kogyo: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal