Abstract
Background
Rituximab in combination with chemotherapy has been shown to improve overall survival (OS) in pts with FL compared with chemotherapy alone. The effect of MR was evaluated in randomized clinical trials (RCTs) with conflicting results regarding OS. In a previous systematic review and meta-analysis of summary (aggregate) data we demonstrated an OS benefit of MR treatment in pts with relapsed or refractory FL and an improved progression free survival (PFS) in both untreated and relapsed refractory FL. However, pts' disease and treatment characteristics may interact with the effect of MR.
To improve identification of sub-groups of pts who may benefit from MR treatment, and to evaluate factors that interact with the effect of MR we conducted an international IPD (raw data) meta-analysis of RCTs of MR for pts with FL. We present the first analysis of this meta-database.
Methods
In June 2014, we updated an electronic search in Pubmed and the Cochrane Library, conference proceedings and database of clinical trials for randomized trials comparing MR to observation. The investigators of eleven trials that fulfilled inclusion criteria were invited to cooperate. Results of one trial were not reported and this trial could not be included in the meta-analysis. Seven study groups participated in this collaborative project and contributed data on individual pts, including disease characteristics, past treatment, response, survival and adverse events. We examined the effect of pt, disease and treatment characteristics by performing a series of Cox regression analyses stratified by trial. In a sensitivity analysis we combined the assessed log hazard ratios (HR) using a log-rank test for each study and combined the results using a fixed effect meta-analysis.
Results
We obtained data for 2323 patients randomized in 7 trials of MR compared to observation after induction therapy. The median follow up ranged from 28-114 months. The median age was 57 years (23 - 85 years), and 41% were older than 60 years. 50% of pts were women, 97% had WHO performance status 0-1; 1195 (53%) pts received CHOP/RCHOP, 453 (20%) CVP/R CVP; 1755 (77%) received rituximab containing induction; 33% of pts received 1st induction, 67% ≥2nd.
Overall, pts less than 60 years of age (vs. ≥60 years) (p < 0.0001), and women (p = 0.001) had a better prognosis. There was no interaction between sex and the effect of MR (p = 0.65).
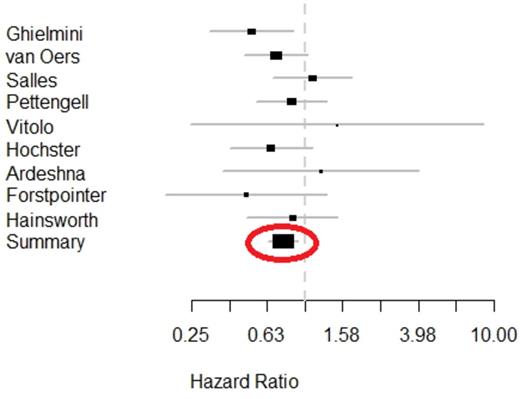
Pts treated with MR had an improved OS compared to observation (HR 0.76, 95% CI 0.62-0.93, p=0.008, Figure). This was demonstrated also in a sensitivity analysis of 10 studies fulfilling inclusion criteria. There was no statistically significant heterogeneity of treatment effect between trials (p=0.15).
In an analysis by treatment line (1st vs. ≥2nd), the estimated effect of MR among patients who received ≥2nd induction was HR of 0.70 (95% CI 0.55 - 0.91), compared to 0.90 (95% CI 0.65 - 1.25) among patients who received 1st induction. However, this difference was not statistically significant (p=0.25). Analysis by the inclusion of rituximab in induction demonstrated among patients who received rituximab in induction a HR of 0.82 (95% CI 0.63 – 1.06), and among those who received induction without rituximab a HR of 0.68 (95% CI 0.49 – 0.93). This difference was not statistically significant (p= 0.35). Analysis by chemotherapy regimen demonstrated an estimated effect for MR among patients who received RCHOP/CHOP of 0.79, 95% CI 0.58 – 1.06, and after RCVP/CVP of 0.65, 95% CI 0.42 – 1.02, with no statistically significant difference between these sub-groups (p = 0.50).
Conclusions
This is the first report of the collaborative group of maintenance therapy for FL patients. Based on individual patient data, this study demonstrated an improved OS with MR therapy for patients with FL. A sensitivity analysis with all 10 eligible trials supported these results. Results support the effectiveness of MR among patients after their 1st induction as well as after ≥2nd induction, and irrespective of inclusion of rituximab in induction, and the chemotherapy regimen. These results are consistent with those of the summary data meta-analysis that was previously published. The wider CI and lack of statistical significance within sub-groups could be attributed to the sample size.
Pooled HR of death of MR compared to observation in patients with follicular lymphoma. In one study there were no events in one group and it is not represented in the forest plot.
Pooled HR of death of MR compared to observation in patients with follicular lymphoma. In one study there were no events in one group and it is not represented in the forest plot.
Vidal:Roche: unrestricted grant Other. Shpilberg:Roche: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal