Abstract
Background.
Fanconi anemia (FA) is a rare, phenotypically heterogeneous, inherited disorder clinically characterized by congenital abnormalities, progressive bone marrow failure (BMF) and a predisposition to develop malignancies. Hematopoietic stem cell transplantation (HSCT) is the only curative option for FA patients. However, finding the best conditioning regimen is still challenging for clinicians. To reduce toxicities, we used progressively lower doses of cyclophosphamide (CY) for conditioning through non-irradiation based regimens. A reduced conditioning regimen based on CY 60mg/kg alone was proposed by Bomfim et al (BBMT, 2007). Survival rates were excellent but some patients experienced primary (n=1) or late (n=4) graft failure (11% of the patients). Mucositis was a major problem as 25 patients (60%) presented grade 3 / 4 mucositis. The rate of Chronic graft versus host disease (GvHD) was 29%. We hypothesized that tapering the dose of CY to 40mg/Kg and adding fludarabine (FLU) at 90mg/m2 might improve engraftment, decrease GvHD rates and eventually improve overall toxicity in FA patients transplanted with HLA matched siblings.
Method.
In 2004, the French reference centre for aplastic anemia and the French Society of Bone Marrow Transplantation and Cell Therapies (SFGM-TC) recommended to use FLU 90mg/m2 (30mg/m2 days -4, -3, -2) and CY 40mg/kg (10mg/kg days -5, -4, -3, -2) for FA patients transplanted from matched family donor. Indication for transplantation was based on hematological complications (transfusions and/or infections). FA patients with morphologic signs of clonal evolution (myelodysplastic syndrome or acute myeloid leukemia) were excluded. All patients in France who received a first Allo-HSCT for FA from a matched related donor between October 2004 and January 2013 using this approach were analyzed (n=20). Clinical data were prospectively collected using ProMISe (Project Manager Internet Server), an internet-based data registry system shared by all SFGM-TC centres. All patients received uromitexan. Ciclosporin A and micophenolate mofetil were used as GVHD prophylaxis. Six patients received an in vivo T cell depletion using antithymocyte globuline because of local policy at their centre. The guidelines were approved by Saint-Louis hospital ethical committee.
Results.
The median age at transplant was 9 years (range: 6-19). Stem cell source was bone marrow in 16 cases and matched related cord blood in the remaining transplants. None of the patients received peripheral blood stem cells. All patients had severe or moderate BMF (median hemoglobin: 8.9g/dl, median platelets: 31 103/ul, median neutrophils: 0.88 103/ul) at time of transplant. Two patients had chromosomal abnormalities (47,XX,i(1)(q10)[10]/48,idem,+8[3] and 47,XX,+der(1;3)(q10;q10)[14]/46,XX[6]); however, none of them developed overt myelodysplasia/leukemia before transplant. Patients belonged to complementation groups FANC-A (n=17) and FANC-G (n=2). Transplantation was performed within a median of 30 months from FA diagnosis (range: 7-143). A median of 3.8. 108 nucleated marrow cells were infused (range: 0,65-8,97).
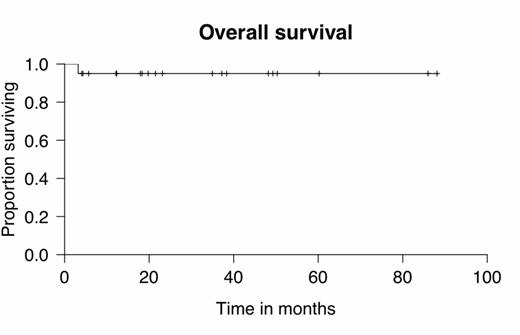
Within a median follow up of 2 years (range: 0.2-7.4), overall survival was 95% (figure 1). Only one patient with an atypical form of FA associated with severe immunodeficiency prior to transplant died subsequently due to uncontrolled cerebral toxoplasmosis. Engraftment rate was 100% with a median time to neutrophils and platelets recovery of 16.5 (11-28) and 15 (4-29) days, respectively. No grade 3/4 regimen related toxicity was observed and only 1 patient experienced mucositis (grade 2) using this conditioning regimen. Total acute GvHD grade 3 / 4 was only observed in 3 patients (15%) and chronic GvHD was extensive in 2 patients (10%) and limited in 3 patients (15%). Median alive patients karnofsky scored 100% (range 90 – 100%). No secondary malignancy was observed in our cohort so far.
Conclusion.
The combination of low dose CY (40mg/Kg) plus FLU (90mg/m2) in HLA-matched donor HSCT in patients with FA resulted in an excellent engraftment rate (100%) with no secondary graft failure, low rates of acute and chronic GvHD, low rates of regimen related toxicity, eventually resulting in an excellent overall survival (95% at 2 years). A longer follow-up in this cohort is needed to confirm such excellent results long-term, namely the continued absence of secondary cancer.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal