Abstract

Backgrounds: Allo-immunization to blood cell antigens has been frequently reported among transfusion recipients with hematological diseases and cancer, as well as during pregnancy. The frequency of irregular erythrocyte antibodies (Abs) ranges from 1 to 2 % among hospitalized patients. However, the frequency varied according to the genetic diversity of the population. Several studies involving transfusion cases have been conducted in various countries including Japan (Watanabe et al, ASH 2009). However, there is currently little information about irregular erythrocyte Abs in many Asian populations. Here, we show updated data concerning variations of irregular erythrocyte Abs in patients with a history of blood transfusions between South Korea and Japan.
Materials and Methods: In all, 21 institutions from South Korea and 59 from Japan participated in this study. We investigated methods employed for screening and identifying irregular erythrocyte Abs. The frequencies of irregular Abs to D, C, c, E, e, f, Ce, P1, M, N, S, s, Mia, Lea, Leb, Jka, Jkb, Jk3, Fya, Fyb, K, k, Kpa, Kpb, Jsa, Jsb, Dia, Dib, Lua, Lub, Xga and H were studied. If a case was analyzed multiple times, it was counted once. Multiple antibodies detected in the same patient were counted separately. The frequencies of irregular erythrocyte Abs on the basis of blood transfusion history were analyzed and compared between patients from South Korea and Japan. We partially selected irregular erythrocyte Abs detected in patients that were initially negative before receiving a transfusion. Among them, we compared the efficacy of detection methods between the indirect antiglobulin test (IAT) and the enzyme method at the first detection of the Abs.
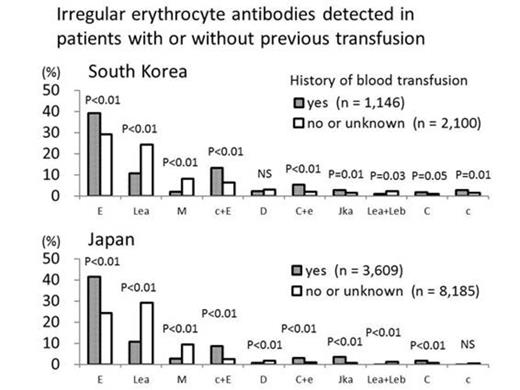
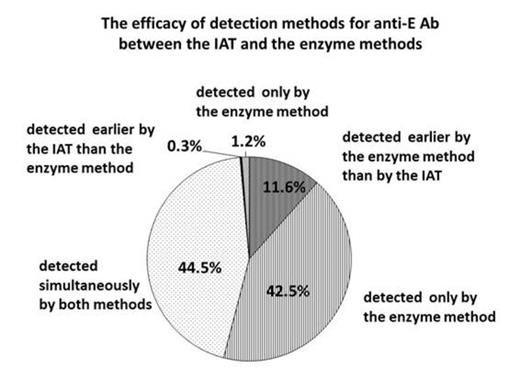
Results: In total, antibodies were detected in 16,438 patients (3,525 from South Korea; 12,913 from Japan). The female to male ratios of patients from the South Korean and Japanese institutions were 1.53 and 1.43, respectively. The number of patients with and without a history of previous transfusion was 1,146 and 2,100 in South Korea, 3,609 and 8,185 in Japan, respectively. Anti-E (1.4x, p<0.01 in South Korea; 1.7x, p<0.01 in Japan), anti-C (1.8x, p=0.05 and 2.3x, p<0.01, respectively) and anti-Jka (1.8x, p=0.01 and 5.8x, p<0.01, respectively) were frequently detected in patients who had received blood transfusions in either country. Anti-c was 1.8 times more frequently detected in patients who had received transfusions in South Korea, but there was no significant increase observed in patients who had received transfusions in Japan. Anti-D did not increase in patients who had received a transfusion in either country. Anti-c+E (2.1x in South Korea and 3.4x in Japan), anti-C+e (2.6x and 3.2x, respectively) and anti-E+Jka (9.2x and 6.3x, respectively) complex Abs increased in patients who had received a blood transfusion. Anti-E was newly detected in 341 patients after receiving a blood transfusion. In 40 cases, anti-E was detected earlier by the enzyme method than by the IAT method. In 147 cases, anti-E was detected only by the enzyme method; while in 4 cases detection was confirmed only by the IAT procedure. Anti-E was simultaneously detected in 154 cases by both methods.
Conclusion: The data presented in this study was derived from a collaboration between South Korea and Japan on alloimmunity to erythrocyte antigens. The total number of positive cases was more than 16,000. Anti-E, anti-C, anti-Jka, anti-c+E and anti-C+e were frequently detected among patients with a history of previous blood transfusions. These results were similar between South Korean and Japanese patients. Anti-c was frequently detected in transfused patients from South Korea, but the number of positive cases did not change in Japanese patients who had undergone a transfusion. These observations might be explained by the ethnic difference in allo-immunity among patients or detection methods adopted in the various participating institutions. Further data, including details of the detection method, will be analyzed in future studies.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal