Abstract
Background: Vascular thromboembolism (VTE) is a recognized complication of cancer. Clinical trials have demonstrated varying degrees of efficacy of antithrombotic agents in preventing VTE in patients suffering from cancer. Benefit of anticoagulants was found to be more pronounced among patients who are at a higher risk for VTE such as patients with advanced cancer and patients undergoing chemotherapy and/or radiotherapy. However, the optimal dose of anticoagulants used in these settings remains unknown. Therefore, we have performed a systematic review and meta-analysis of randomized controlled trials (RCT) to evaluate the efficacy of different dosing of anticoagulants in the primary prevention of VTE among patients with advanced solid malignancies receiving chemotherapy.
Methods: We undertook an extensive electronic database search using PUBMED and EMBASE databases for eligible studies. RCTs, involving patients with advanced solid malignancies receiving chemotherapy, which reported VTE rates as a primary or secondary outcome were included. RCTs that had a mixed population of patients such as all stages of cancer, solid and hematologic cancers, and chemotherapy and non-chemotherapy patients were excluded. The primary outcomes in this analysis were all reported VTE events and major bleeds. The secondary outcome was overall mortality rate. We used Comprehensive Meta-analysis Version 2 (Biostat, Englewood NJ) to estimate the pooled event-based risk ratio (RR) and risk difference (RD) with 95% confidence interval (CI) by using Mantel-Haenszel method. Random effects model was applied because of heterogeneity among the studies.
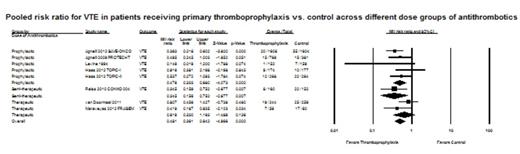
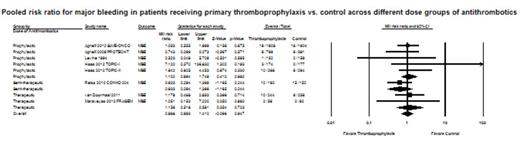
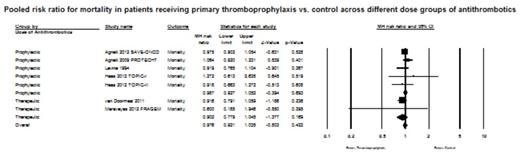
Results: Eight RCTs comprising 6,492 patients (5 RCTs using prophylactic dose (n = 5,556), 1 RCT using semi-therapeutic dose (n = 312), 2 RCTs using therapeutic dose (n = 624)) are eligible for analysis. The duration of thromboprophylaxis ranged from 6 weeks to 6 months. The crude VTE rates were 2.65% and 5.66% in thromboprophylaxis and control groups, respectively, with an overall RR of 0.48 (CI = 0.36 – 0.64). RRs for VTE in patients receiving prophylactic, semi-therapeutic and therapeutic doses of anticoagulants were 0.48 (CI = 0.33 – 0.68), 0.35 (CI = 0.16 – 0.75) and 0.62 (CI = 0.33 – 1.16), respectively. The RRs of these subgroups were not significantly different from one another (p = 0.518). The overall RD was -0.024 (CI = -0.033 – -0.016), suggesting an estimated number needed to treat (NNT) of 42 (CI = 30 – 63) to prevent one VTE event. RRs for major bleeding across different antithrombotic doses were not statistically different (p = 0.44) with RRs of 1.1 (CI = 0.69 – 1.75), 0.63 (CI = 0.29 – 1.37) and 1.16 (CI = 0.52 – 2.58) for prophylactic, semi-therapeutic and therapeutic doses, respectively. The overall RR for major bleeding was 0.99 (CI = 0.69 – 1.41). There was no difference in mortality rate between thromboprophylaxis and control groups (RR = 0.98, CI = 0.92 – 1.04, p = 0.42). However, there was a nonsignificant trend towards improvement in mortality in the therapeutic dose subgroup (RR = 0.9, CI = 0.78 – 1.05, p = 0.17).
Conclusions: Our meta-analysis demonstrated that, among patients with advanced solid malignancies receiving chemotherapy, primary thromboprophylaxis with anticoagulants significantly reduced VTE events without an increase in major bleeding events compared to control, even though an overall survival benefit was not observed. The benefit in VTE reduction, the risk of major bleeding events and the incidence of overall mortality were similar among the three dosing regimens. However, it was noted that there was a nonsignificant trend towards survival advantage in the therapeutic dose subgroup.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal