Abstract
Introduction: High-density lipoprotein (HDL) protects against thromboembolic coronary disease via reverse cholesterol transport mediated by HDL's primary lipoprotein subunit, apolipoprotein A-I (apoA-I), binding to scavenger receptor BI (SR-BI). Absence of SR-BI increases platelet aggregation and venous/arterial thrombosis in mice, consistent with an antithrombotic role of this signaling axis. To date, the effects of the isolated apoA-I subunit on platelet activation remain unknown. We hypothesize that the antithrombotic effect is mediated by apoA-I signaling through platelet-specific SR-BI.
Methods: Platelet function assays were performed on samples from healthy human volunteers (n=3). ApoA-I levels were determined using an ELISA kit. Microfluidic analysis of platelet aggregate formation on collagen under physiologic flow conditions (650 sec-1) was carried out in whole blood samples. Light transmission platelet aggregation in response to collagen and ristocetin was conducted using both platelet rich plasma (PRP) and washed platelets (WP). Venous and arterial thromboses were induced in wild type C57Bl/6 mice in a collagen (0.3 mg/kg)/epinephrine (0.03 mg/kg)-induced pulmonary embolism model and a 6% ferric chloride (FeCl3)-induced carotid artery thrombosis model, respectively. Recombinant human apoA-I was used with a final concentration of 300 µg/mL.
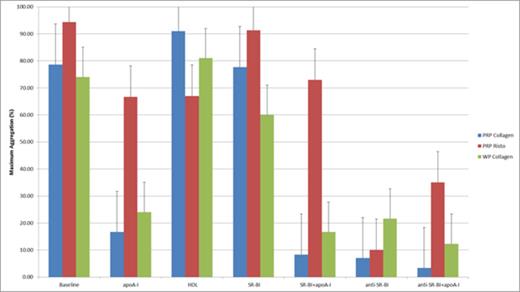
Results/Discussion: ApoA-I plasma levels in the subjects studied fell within previously published ranges. Microfluidic analysis of platelet aggregate formation on collagen under shear stress did not demonstrate significant difference in total surface area coverage (n=3 in quadruplicate), but apoA1-treated samples demonstrated a significantly greater proportion of small aggregates (3-10 platelets/aggregate, 40.2% vs 31.8%, p<0.0001), compared to controls which had a significantly greater proportion of large aggregates (51-100 plts/agg, 6.3 vs 2.3%, p<0.001 and >100 plts/agg, 2.3% vs 0.7%, p<0.05). Platelet aggregation studies (Fig. 1) revealed significantly decreased collagen-induced aggregation in platelets treated with apoA-I compared to vehicle-treated controls in both PRP and WP samples, suggesting direct action of apoA-I on platelets. The difference was less pronounced in ristocetin-induced aggregation, though still significant, consistent with decreased activation of VWF, which has been recently shown to bind apoA-I. Apoa-I-treated PRP samples also had significantly decreased dense granule (ATP) release compared to non-treated samples. Pre-treatment with native HDL had no significant effect, consistent with studies demonstrating that only oxidized HDL inhibits aggregation. Recombinant human SR-BI (rhSR-BI) alone had little effect in PRP but inhibited collagen-induced aggregation in WP. Addition of rhSR-BI and apoA-I together inhibited aggregation in both PRP and WP to a greater degree than either component alone. Rabbit anti-human SR-BI alone had little effect in PRP but inhibited collagen-induced aggregation in WP. FeCl3 applicationinduced initial arterial occlusion within 8.8 +/-0.8 minutes in apoA-I-treated mice treated (n=3) compared to 6.1 +/- 0.3 minutes in vehicle-treated controls (n=3, p<0.01, t-test). Systemic thrombosis resulting in pulmonary embolism was induced by injection of collagen/epinephrine. Median time of survival after injection in mice pre-treated with apoA-I (n=5) was 30 +/- 0 minutes, compared to 3.3 +/- 0.4 minutes in vehicle-treated controls (n=5, p<0.001, t-test). Experiments were stopped after 30 minutes, at which time all apoA-1-treated mice were still alive, compared to zero controls.
Conclusion: Though the mechanism is not yet completely understood, the data show an inhibitory effect of isolated human apoA-I on human platelet activation and murine arterial/venous thrombosis, likely through platelet inhibition. The increased inhibition seen with rhSR-BI and apoA-I together is consistent with previous studies demonstrating SR-BI's regulatory role in platelet function. Ongoing studies include increasing sample size for human platelet function assays and murine venous/arterial thrombosis models in wild type mice with and without infusion of apoA-I compared to SR-BI-/- and apoA-I-/- mice with and without infusion of apoA-I.
Maximum aggregation values (mean +/- SEM) following addition of collagen or ristocetin
Maximum aggregation values (mean +/- SEM) following addition of collagen or ristocetin
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal