Abstract

Background
Hematologic toxicity is a common treatment complication of chronic hepatitis C virus (HCV) infection, especially when interferon (IFN) and ribavirin are used. The side effects of treatment are often augmented in cancer patients due to baseline cytopenias. These adverse events often lead to dose reduction or discontinuation of antivirals. Hematopoietic growth factors (GF) and blood transfusions are used to counteract toxicities allowing patients to complete treatment. We aimed to evaluate the incidence and management of hematological toxicity associated with different types of HCV treatment in cancer patients.
Methods
Medical records of cancer patients treated for HCV infection at MD Anderson Cancer Center between 2009 and 2014 were reviewed. Those seen from 8/2009 to 10/2012 were analyzed retrospectively, whereas those seen from 11/2012 to 7/2014 were prospectively studied. Patients who received combination treatment with peg-IFN and ribavirin (PR), telaprevir or boceprevir plus PR (TBPR), sofosbuvir plus PR (SPR), sofosbuvir with simeprevir (SS) and sofosbuvir with ribavirin (SR) were included in the study. Data regarding treatment interventions (dose reductions and/or discontinuation of antivirals), use of GFs or blood transfusions in the management hematological side effects were analyzed. Categorical variables were analyzed using the χ2 or Fischer's exact test.
Results
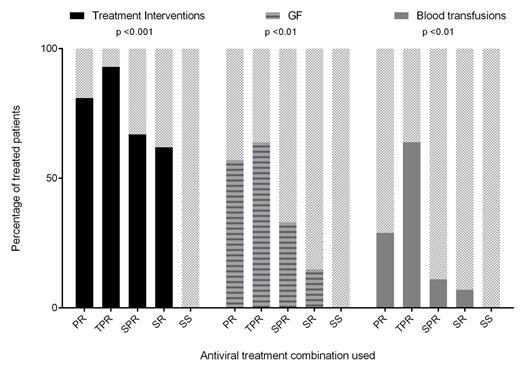
Sixty-five patients were identified (Table). The need for treatment interventions, GFs or blood transfusions was comparable between patients with hematologic malignancies and solid tumors. Seventeen (81%) of the PR group, 13 (93%) of the TBPR group, 6 (67%) of the SPR group, 9 (64%) of the SR group and 0 of the SS group required treatment interventions (p <0.001) (Figure). Twelve (57%) of the PR group, 9 (64%) of the TBPR group, 3 (33%) of the SPR group, 2 (14%) of the SR group and 0 of SS group required the use of GFs (p <0.01). Six (29%) patients of the PR group, 9 (64%) from the TBPR group, 1 (11%) from the SPR group, 1 (7%) from the SR group and 0 from the SS group received blood transfusions (p <0.01). From patients who received GFs (N=26), 2 received epoetin alfa, 11 darbepoetin alfa, 2 filgrastim, 17 pegfilgrastim, 4 eltrombopag and 1 romiplostim. Ten of them (39%) required multiple GFs, with darbepoetin alfa and pegfilgrastim being the most common combination. Combined use of GFs was only needed in those receiving TBPR (56%), PR (33%) or SPR (33%). Overall, 82% of the patients who received treatment interventions, 77% of those who received GFs and 47% of those who received blood transfusions were able to complete HCV treatment. Thirteen patients (62%) from the PR group, 12 (86%) from the TBPR group, 3 (33%) from the SPR group, 2 (14%) from the SR group and 0 from the SS group developed grade 3 or 4 hematologic toxicities (p <0.001). One (25%) of 4 patients receiving eltrombopag developed portal vein thrombosis. No other patients developed side effects attributed to GF support.
Conclusions
Hematologic toxicity during HCV treatment in cancer patients is common. The use of GFs helps manage such toxicity, allowing completion of antiviral therapy. The newer HCV direct-acting antiviral agents are associated with less hematological toxicity, requiring fewer interventions, GFs and blood transfusions. No hematologic side effects were seen with the IFN-free, ribavirin-free combination of SS.
Characteristics of HCV-infected cancer patients treated with different antiviral regimens
| . | PR (N=21) % . | TBPR (N=14) % . | SPR (N=9) % . | SR (N=14) % . | SS (N=7) % . |
|---|---|---|---|---|---|
| Age, median (range) | 54.3 (45-68) | 59.7 (49-69) | 54.7 (35-75) | 62.7 (33-82) | 60.9 (46-64) |
| Male gender | 13 (62) | 6 (43) | 4 (44) | 8 (57) | 4 (57) |
| Type of cancer Solid Hematologic | 16 (76) 5 (24) | 10 (71) 4 (29) | 4 (44) 5 (56) | 6 (43) 8 (57) | 4 (57) 3 (43) |
| Cirrhosis | 5 (24) | 7 (50) | 2 (22) | 3 (21) | 6 (86) |
| Baseline labs, median (range) Hemoglobin (g/dL) Platelets (x1,000 K/uL) Absolute Neutrophil count (K/uL) | 12.8 (10-15.9) 165 (83-408) 1385 (940-6120) | 13.5 (9.6-16.3) 112 (52-397) 2360 (800-4900) | 13.8 (8.8-14.2) 183 (121-268) 2680 (1650-5810) | 13.1 (9.8-15.5) 179 (57-390) 2490 (1040-4040) | 13.8 (12.3-16.1) 141 (59-239) 3000 (1390-5030) |
| FDA-recommended duration of antiviral treatment, weeks | 24-48 | 24-48 | 12 | 12-24 | 12 |
| Duration of antiviral treatment, median (range) | 24 (2-48) | 19 (3-52) | 12 (1-12)* | 12 (3-24)* | 6 (3-12)* |
| . | PR (N=21) % . | TBPR (N=14) % . | SPR (N=9) % . | SR (N=14) % . | SS (N=7) % . |
|---|---|---|---|---|---|
| Age, median (range) | 54.3 (45-68) | 59.7 (49-69) | 54.7 (35-75) | 62.7 (33-82) | 60.9 (46-64) |
| Male gender | 13 (62) | 6 (43) | 4 (44) | 8 (57) | 4 (57) |
| Type of cancer Solid Hematologic | 16 (76) 5 (24) | 10 (71) 4 (29) | 4 (44) 5 (56) | 6 (43) 8 (57) | 4 (57) 3 (43) |
| Cirrhosis | 5 (24) | 7 (50) | 2 (22) | 3 (21) | 6 (86) |
| Baseline labs, median (range) Hemoglobin (g/dL) Platelets (x1,000 K/uL) Absolute Neutrophil count (K/uL) | 12.8 (10-15.9) 165 (83-408) 1385 (940-6120) | 13.5 (9.6-16.3) 112 (52-397) 2360 (800-4900) | 13.8 (8.8-14.2) 183 (121-268) 2680 (1650-5810) | 13.1 (9.8-15.5) 179 (57-390) 2490 (1040-4040) | 13.8 (12.3-16.1) 141 (59-239) 3000 (1390-5030) |
| FDA-recommended duration of antiviral treatment, weeks | 24-48 | 24-48 | 12 | 12-24 | 12 |
| Duration of antiviral treatment, median (range) | 24 (2-48) | 19 (3-52) | 12 (1-12)* | 12 (3-24)* | 6 (3-12)* |
*Patients may still be on treatment.
Management of hematologic toxicity during HCV treatment of cancer patients
Torres:Genentech,: Consultancy; Vertex Pharmaceuticals: Consultancy, Research Funding; Merck & Co., Inc. : Consultancy, Research Funding; Gilead Sciences: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal