Abstract
Background:
The increased risk of acute vaso-occlusive pain crisis and splenic infarction in children with sickle cell disease (SCD) acutely exposed to altitude has been well documented. However, little is known about complication rates in children chronically living at moderate altitude. We hypothesize that children with SCD experience more complications than children with SCD living at sea level.
Methods:
A retrospective chart review of all patients with sickle cell disease followed at the Children's Hospital Colorado between January 2001 and December 2010 was completed. Patients observed for less than one year were excluded from analysis. Incidence rates for vaso-occlusive crisis (VOC), acute chest syndrome (ACS), splenic sequestration, and stroke were calculated. Rate ratios and 95% confidence intervals were determined comparing to children with SCD from institutions located near sea level. Secondary measures looked at baseline hematologic indices collected at annual comprehensive care visits and percentage of patients with abnormal tricuspid regurgitation jet velocity (TRV). Two-tailed Student's t-tests were used to compare means of continuous variables.
Results:
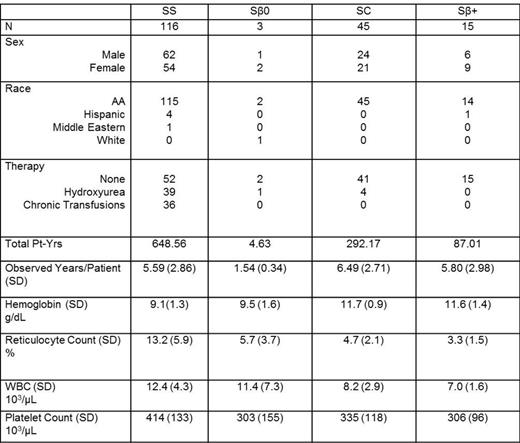
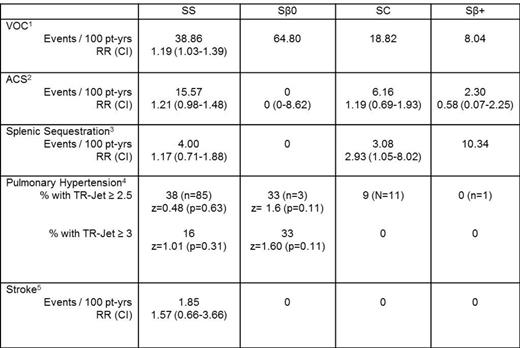
179 children were observed for a total of 1032.37 patient-years with demographics (Table 1). . At moderate altitude, patients with Hgb SS experienced about a 20% higher rate of VOC compared to historic controls with a rate ratio of 1.19 (1.03-1.39) (Table 2). Patients with Hgb SC had almost 3 times the number of admissions for splenic sequestration than those at sea level with a rate ratio of 2.93 (1.05-8.02). Incidence rates for ACS and stroke appeared to have been higher at moderate altitude than sea level, but did not reach statistical significance. There was also no difference in the percentage of patients with abnormal TRV. Baseline lab values were less than the 95%ile except for the hemoglobin of 11.7 for SC patients (Brown et al 1994).
Discussion:
The oxygen tension at an elevation of 5,280 feet (1,609 m) is 20% lower than at sea level due to the reduction in barometric pressure. Reduced oxygen tension may lead to increased hemoglobin S polymerization and red cell sickling. Hemoglobin SC patients have higher baseline hemoglobins, and their increase in splenic sequestration may be due to increased blood viscosity. Interestingly, the rate of ACS and pulmonary hypertension did not seem to be significantly elevated in our patients living at moderate altitude. This may be due to a lack of statistical power given the small size of this single institution study. Another limitation of this study is the comparison to data from multiple institutions near sea level which does not necessarily control for other possible contributing factors, e.g. climate. Also, VOC events were defined as hospitalizations requiring parenteral opioid administration, which is a stricter definition than used in the sea-level data. Thus, the risk ratio may be underestimated. Nevertheless, the data supports the anecdotal experience that patients living chronically at moderate altitude have increased sickle cell-related complication rates.
1 -compared to Gill et. al, Blood, 1995
2 - compared to Vichinsky et. al, Blood, 2012
3- compared to Brousse et. al, BJH, 1997
4- compared to Pashankar et. al, Pediatrics, 2007
5- compared to Quinn et. al, Blood, 2008
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal