Abstract
Introduction: Endothelial function is impaired in sickle cell anemia (SCA) and may be prognostic of severity of pathophysiology underlying many complications. Poor nutritional status is documented in SCA in all income settings, yet no strategies exist to improve nutrition. Poor nutritional status and hemoglobin predict death and hospitalization in Tanzanian SCA patients (Cox, et al. Haematologica 96, 2011, Makani et al. PloSONE 6, 2011). The objectives are to determine the combined effect of two ready-to-use-supplementary food (RUSF) interventions on the primary endpoints of endothelial function, assessed by flow mediated dilatation (FMD), growth and body composition and hemoglobin (secondary endpoint).
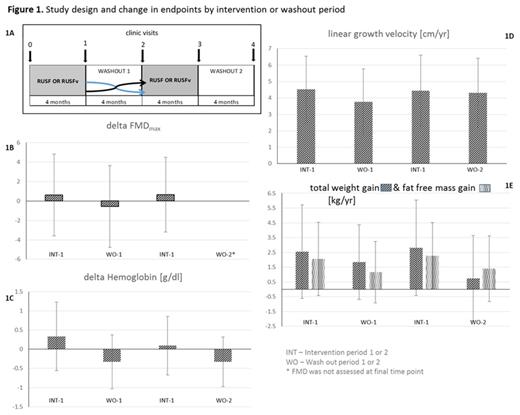
Methods: Tanzanian children (N=119) (HbSS) aged 8-11.9 years were enrolled in V-FIT (ISRCTN74331412/NCT01718054) in Aug to Nov 2012. Children received in random order a daily RUSF providing 500 kcal, 1 RDA of vitamins and minerals & 1mg folate (Nutriset, France), plus weekly anti-malarial prophylactic chloroquine syrup (150/225mg base) (Wallace manufacturing chemicals, UK), or a vascular-RUSF (RUSFv) fortified with arginine and citrulline (average 0.2g/kg/d & 0.1g/kg/d) plus daily chloroquine syrup (3mg base/kg/d). Patients and investigators were blind to the different interventions. Each intervention was received for 4 months with 4 month washout periods on either side (Figure 1A). Clinic visits were conducted at baseline and at the end of each intervention/washout period when endothelium-dependent and -independent vasodilatation were assessed (Donald et al. JACC 51, 2008), plus height, weight and body composition by impedance (Tanita BC418). Random effects models were used, adjusting for repeated measures within individuals. In multivariable analyses models were a priori adjusted for gender. Possible temporal effects were modelled via Fourier transformation of visit dates and included in models for growth and hemoglobin. Effects of the interventions on FMDmax were adjusted for arterial diameter before vasodilation induction, which was negatively correlated with FMDmax and for magnitude of reactive hyperaemia during induction of vasodilation, which was not correlated with FMDmax.
Results: 115/119 (60% male; mean age at enrolment 10.0, 95% CI 9.8 – 10.2 years) enrolled patients completed the trial and all clinic visits. Endpoints at baseline and the adjusted and unadjusted effects of the interventions are shown in Table 1. FMDmax, baseline brachial diameter, absolute change in blood flow velocity during reactive hyperemia, hemoglobin, height velocity, weight and lean mass gain all increased on the RUSF (Fig 1B-F).
Discussion: We demonstrate that providing extra protein, energy and micronutrients improves hemoglobin, vascular endothelial function and growth. It is possible that the effects observed are limited to the RUSFv, and/or from unadjusted for temporal effects. Unblinded analysis of the effect of RUSFv vs. RUSF on these endpoints, plasma amino acids and arginase are planned. Currently the only intervention for children with SCA is hydroxyurea, which although it improves hemoglobin and reduces hemolysis, does not appear to affect growth while its effect on vascular physiology is unknown (Wang et al. J Pediatr 140, 2002). In addition to specific nutrients, general improvement in nutrition may result in improvement in important intermediate endpoints in SCA. Future research should investigate effects of nutritional supplementation on clinical endpoints.
Endpoints at enrolment and combined effect of RUSF interventions.
| . | Baseline N=119 . | RUSF coefficient [95% CI] . | P-value . | Adjusted RUSF coefficient [95% CI] . | Adjusted P-value . |
|---|---|---|---|---|---|
| Endothelial function, mean [SD] | |||||
| FMDmax % | 7.66 [3.37] | 0.66 [0.15 – 1.17] | 0.011 | 0.98 [0.42 – 1.54] | 0.001 |
| Baseline brachial diameter, mm | 2.61 [0.35] | 0.05 [0.03 – 0.09] | <0.001 | - | - |
| Reactive hyperemia absolute, m/s | 0.69 [0.22] | 0.034 [0.004 – 0.065] | 0.026 | - | - |
| Anemia, mean [95% CI] | |||||
| Hemoglobin, g/dl | 7.5 [7.3 – 7.7] | 0.29 [0.20 – 0.37] | <0.001 | 0.34 [0.22 – 0.46] | <0.001 |
| Anthropometry, mean [95% CI] | |||||
| Height cm | 126.5 [125.2 – 127.8] | - | - | - | - |
| Linear growth velocity, cm/yr | - | 0.46 [0.08 – 0.83] | 0.018 | 0.51 [0.01 – 1.02] | 0.053 |
| Weight, kg | 22.8 [22.1 – 23.5] | - | - | - | - |
| Weight gain, kg/yr | - | 1.37 [0.83 – 1.91] | <0.001 | 1.98 [1.25 – 2.73] | <0.001 |
| Whole body fat free mass, kg | 18.6 [18.1 – 19.1] | - | - | - | - |
| Fat free mass gain, kg/yr | - | 0.89 [0.48 – 1.30] | <0.001 | 0.93 [0.36 – 1.50] | 0.001 |
| . | Baseline N=119 . | RUSF coefficient [95% CI] . | P-value . | Adjusted RUSF coefficient [95% CI] . | Adjusted P-value . |
|---|---|---|---|---|---|
| Endothelial function, mean [SD] | |||||
| FMDmax % | 7.66 [3.37] | 0.66 [0.15 – 1.17] | 0.011 | 0.98 [0.42 – 1.54] | 0.001 |
| Baseline brachial diameter, mm | 2.61 [0.35] | 0.05 [0.03 – 0.09] | <0.001 | - | - |
| Reactive hyperemia absolute, m/s | 0.69 [0.22] | 0.034 [0.004 – 0.065] | 0.026 | - | - |
| Anemia, mean [95% CI] | |||||
| Hemoglobin, g/dl | 7.5 [7.3 – 7.7] | 0.29 [0.20 – 0.37] | <0.001 | 0.34 [0.22 – 0.46] | <0.001 |
| Anthropometry, mean [95% CI] | |||||
| Height cm | 126.5 [125.2 – 127.8] | - | - | - | - |
| Linear growth velocity, cm/yr | - | 0.46 [0.08 – 0.83] | 0.018 | 0.51 [0.01 – 1.02] | 0.053 |
| Weight, kg | 22.8 [22.1 – 23.5] | - | - | - | - |
| Weight gain, kg/yr | - | 1.37 [0.83 – 1.91] | <0.001 | 1.98 [1.25 – 2.73] | <0.001 |
| Whole body fat free mass, kg | 18.6 [18.1 – 19.1] | - | - | - | - |
| Fat free mass gain, kg/yr | - | 0.89 [0.48 – 1.30] | <0.001 | 0.93 [0.36 – 1.50] | 0.001 |
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal