Abstract
Introduction: For patients with relapsed or refractory diffuse large B cell lymphoma (DLBCL), salvage treatment followed by consolidation with high-dose chemotherapy and autologous stem cell transplantation (HD-ASCT) is the standard of care for those with chemosensitive disease, as established by the PARMA and CORAL trials. In the pre-rituximab era, patients with DLBCL experiencing disease progression following HD-ASCT had a dismal prognosis with a median overall survival of 3 months. These early studies demonstrate that early progression following HD-ASCT is the most important predictor of poor outcome. In the rituximab era, there is very little data examining incidence and outcomes of patients with late relapses following HD-ASCT for relapsed/refractory DLCBCL. Therefore, we sought to evaluate survival outcomes in a cohort population of patients relapsing late after HD-ASCT for DLBCL.
Methods: We reviewed consecutive patients who underwent HD-ASCT for biopsy confirmed relapsed or refractory DLBCL between 2001 and 2010 at the University of Rochester James P. Wilmot Cancer Institute. Eligible patients were required to have received rituximab as part of their therapeutic regimen. Survival probability was estimated by the Kaplan-Meier method. Comparisons were made using the X2 test and Fisher's exact test, where appropriate.
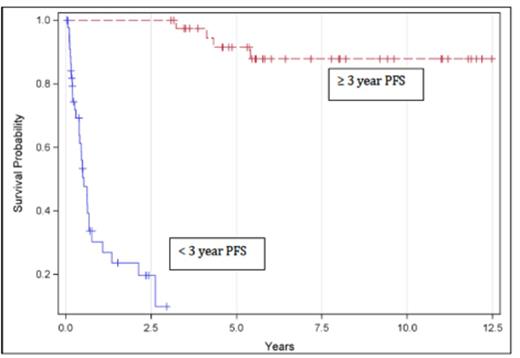
Results: A total of 88 patients were identified. Median age was 55 (range 20-74). Eighty percent of patients received a BEAM – like conditioning regimen (Carmustine, Etoposide, Cytarabine, and Melphalan). Thirty-five patients were in complete remission at the time of transplant. Median follow up for surviving patient was 5.8 years (range 139 days -12.5 years). The median overall survival for all patients was 5.2 years (range of 15 days-12.5 years). In total, 51 patients died (58%); 31 of these deaths were related to DLBCL (61%). Median progression free survival was not reached. Thirty-five patients relapsed following ASCT. Of these, 89% relapsed < 3 years from ASCT (early relapse), 2 of whom remain alive. Only 4 patients (11%) relapsed ≥ 3 years from ASCT (late relapse), 2 of whom died, and 2 of whom remain alive. Of the deaths, 1 was lymphoma-related, and 1 was death from graft versus host disease in a patient undergoing subsequent allogeneic transplant. Median time to progression in the entire cohort was 167 days. Consistent with early studies, the presence of disease status prior to ASCT was associated with shorter time to progression, p=0.0028 by Fisher's exact test.
Conclusions: Ours is one of few series examining late relapses following ASCT performed for relapsed and refractory DLBCL in the rituximab era. In this cohort, late relapses following ASCT for relapsed and refractory DLBCL occurred infrequently. Our data indicate that for the few patients relapsing beyond 3 years, there is a suggestion of long-term disease control.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal