Abstract
Central nervous system (CNS) involvement is considered rare in adults with acute myeloid leukemia (AML). Therefore the cerebrospinal fluid (CSF) is typically examined only in patients with CNS symptoms. In our institution all AML patients considered candidates for allogeneic hematopoietic cell transplantation (HCT) undergo routine CSF examination as part of pre-transplant evaluation, allowing a relatively unbiased look at the incidence of AML in CSF pre-HCT. The primary objectives of this study were to assess the rate of CNS involvement in AML patients undergoing HCT, evaluate potential risk factors for CNS disease, and examine the effect of CNS involvement on transplant outcome.
We retrospectively evaluated 327 adults with AML who underwent ablative HCT between January 2007 and December 2012. Median age was 49 (range 19-73). Twenty eight (8%) patients had favorable karyotype, 215 (66%) had intermediate-risk karyotype, and 84 (26%) had unfavorable karyotype at diagnosis. 206 patients had received a high intensity induction regimen (daily ARA-C dose ≥ 500mg/m2). At time of CSF evaluation pre-HCT, 166 patients were in CR without minimal residual disease (MRD), 65 had CR with MRD, 41 had CRp or CRi, and 54 were in relapse. Median follow-up time was 630 days.
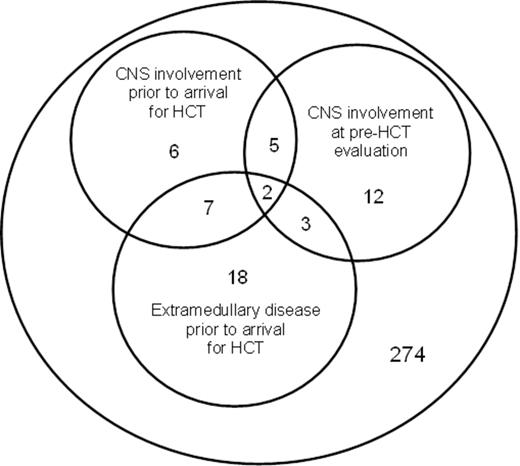
22 patients (7%) had CSF AML involvement, as assessed morphologically or using multiparameter flow cytometry, at their pre-HCT evaluation. 5 of these patients had had prior (treated) CNS AML, 3 had had prior extramedullary disease (EMD) not involving the CNS, and 2 had had both prior CNS and other extramedullary disease (Fig. 1). The incidence of CSF AML at pre-HCT evaluation was 7/20 in patients with past CNS involvement vs. 15/ 307 in patients without history of CNS disease (p <0.001), and was 5/30 in patients with a history of other EMD vs. 17/297 in patients without a history of EMD (p = 0.04). Other covariates associated with CNS AML at pre-HCT evaluation were higher WBC at diagnosis (p <0.001, medians of 34,000 in those with and 5,000 in those without CNS disease) and disease status (p<0.001) with only 2% of patients in CR without MRD had CSF involvement vs. 8% of those with CR with MRD, 7% of those with CRp or CRi, and 19% of those with relapse disease at time of pre-HCT evaluation. Cytogenetics, age, karyotype, and receipt of HiDAC showed no effect on CSF involvement pre-HCT in a univarate analysis.
Classification and regression tree (CART) analysis identified 3 risk groups: (1) high = prior CNS disease (20 pts, 35% with CSF involvement at pre-HCT evaluation), (2) intermediate = no prior CNS involvement but in systemic relapse at pre-HCT CSF evaluation (51 pts, 16% with CSF involvement at pre-HCT evaluation), (3) low = no prior CNS disease and either CR (+/- MRD) or CRp/CRi (254 pts, 3% with CSF involvement at pre-HCT evaluation).
All 22 patients with CSF involvement at pre-HCT evaluation received CNS-directed treatment (intrathecal chemotherapy +/- intracranial irradiation) and cleared their CNS disease prior to transplant. 18 patients also received CNS-directed therapy after HCT (between 1-6 intrathecal treatments). Nine and 8 patients with prior history of CNS disease, but with no evidence of CSF involvement at time of pre-HCT evaluation, received CNS-directed therapy before and after transplant respectively. Two of 35 patients (6%) with CNS disease at any time pre-HCT had documented CNS disease after transplant.
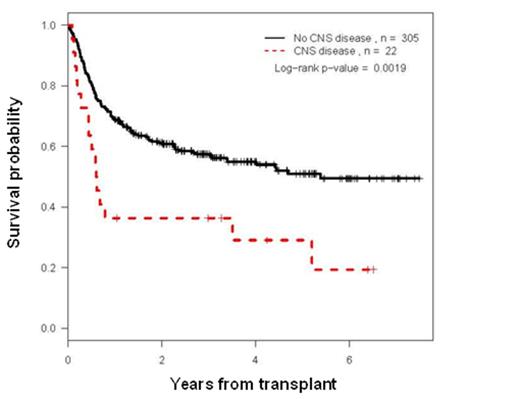
While patients with CSF involvement at pre-HCT evaluation had shorter post-HCT survival (p = 0.002) (Fig. 2), multivariate analysis indicated that this reflected the association of CNS disease with poorer systemic response to therapy and evidence of systemic disease at time of transplant; specifically multivariate hazard rates were 1.48 for CNS involvement vs no CNS involvement (p = 0.17), contrasted with 3.62 for CR with MRD vs CR without MRD (p <0.001) and 3.78 for no CR vs CR without MRD (p <0.001). Tests for interactions indicated that the relatively small effect of CNS disease on survival was similar in patients with CR (+/- MRD), CRp or CRi, or relapse disease at time of CSF evaluation pre-HCT.
We conclude that CNS AML involvement pre-HCT is relatively uncommon (7%), is primarily associated with a history of prior CNS disease, and, when controlled, is not an independent factor in determining survival after HCT.
CNS and extramedullary disease among 327 AML patients undergoing ablative HCT
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal