Abstract
Background: Chronic graft-versus-host disease (cGVHD) is a frequent complication after allogeneic stem cell transplantation (SCT). In its severe form, cGVHD can be a debilitating condition resulting in significant morbidity and increased mortality. However, cGVHD has been associated with reduced relapse rates suggesting that a curative graft-versus-leukemia (GVL) effect concurs with this condition. Preliminary analyses indicate an increased risk of cGVHD in female-> male transplants because of HY minor H antigen mismatching. The aim of this retrospective study was to further explore the effect of donor recipient sex combinations on cGVHD and disease control after SCT for hematopoietic malignancies.
Methods: 424 consecutive patients who received an allogeneic SCT at our institution between 2002 and 2011, consented to participate in this observational study, and survived at least 6 months post SCT were included in this analysis. Median age of patients was 52 years [range 16-70 years], 254 were male. The underlying haematological conditions were acute myeloid leukemia in 126, acute lymphoblastic leukemia 41, myeloproliferative/ myelodysplastic disorders 68, lymphoma 114, and multiple myeloma 75. Transplantation by related donor was performed in 165, by matched unrelated donor in 172, and by mismatched unrelated donor in 87. 396 Patients received peripheral blood stem cells, 28 bone marrow. Myeloablative or aplasia conditioning was administered in 100, reduced intensity conditioning in 324. Chronic GVHD was diagnosed and graded as severe or non-severe applying the National Institutes of Health’s 2005 consensus criteria. Overall survival (OS) and time to relapse were calculated from time of transplantation to death or relapse, respectively, using the Kaplan-Maier method. The impact of various variables on cGVHD risk, survival, and relapse was assessed by univariate log-rank comparisons and multivariate Cox regression.
Results: cGVHD occurred in 215 patients (51%) before relapse, of whom 75 (18%) developed severe cGVHD, and 140 (33%) non-severe cGVHD. Both severe and non-severe GVHD were associated with a significantly prolonged OS compared to non-cGVHD patients (p<.001) due to a reduced relapse rate (p<.001). This effect was stable across all entities. In contrast, no impact on relapse rates could be seen for grade 1-2 or grade 3-4 acute GVHD.
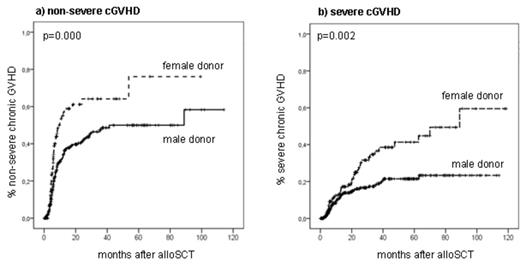
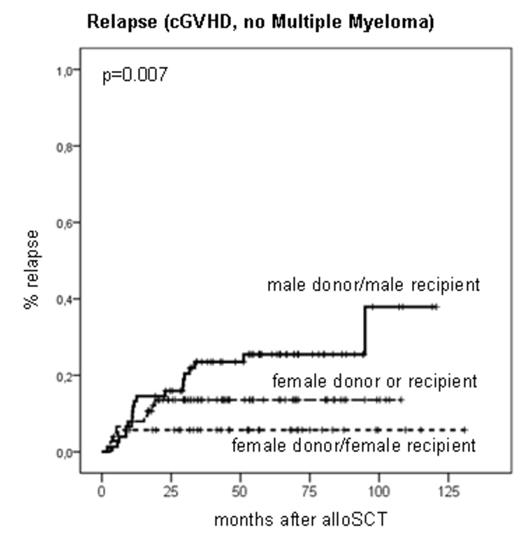
By univariate analysis, the application of anti-thymocyte globuline (ATG) was associated with a significantly reduced cGVHD risk, whilst a female donor significantly increased cGVHD risk, independent of recipient sex and donor pregnancy history (Fig. 1a-b). The increased cGVHD risk of female donors remained significant after multivariate adjustment for ATG, age, recipient sex, stem cell source, diagnosis, and conditioning. Next, the relapse risk among those patients who had any grade of cGVHD was assessed. Apart from the diagnosis multiple myeloma, the donor-recipient constellation male->male was associated with a significantly elevated relapse risk by univariate analysis (p=.007, Fig. 2).
Conclusions: In this single center analysis, female donors were associated with an increased cGVHD risk independent from recipient sex and pregnancy history. Once established, cGVHD resulted in a significantly better disease control (GVL) if donor and/or recipient were female. These observations suggest female sex-related cGVHD and GVL effector mechanisms independent of HY minor Histocompatibility Antigen mismatching which could have major impact on donor selection algorithms but need to be validated and explored by prospective studies.
Incidence of non-severe and severe cGVHD stratified for donor sex.
Incidence of relapse in cGVHD patients (no Multiple Myeloma) stratified for donor and recipient sex.
Incidence of relapse in cGVHD patients (no Multiple Myeloma) stratified for donor and recipient sex.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal