Abstract
Introduction: Graft-versus-host disease (GVHD) is a major cause of treatment failure in allogeneic hematopoietic cell transplantation (HCT). The hematopoietic cell transplant-specific comorbidity index (HCT-CI) predicts transplant-related mortality (Sorror, et al: Blood, 2005; Raimondi, et al: Blood, 2012), but its prognostic value has not been well explored in the setting of GVHD. It is hypothesized that patients with a high HCT-CI score would have worse outcomes after developing GVHD compared to those with a low HCT-CI score. In this retrospective study we calculated the pre-transplant HCT-CI and analysed its relationship with GVHD specific survival (GSS).
Methods: A total of 541 patients who received allogeneic HCT at Princess Margaret Cancer Centre between 2000 and 2012 were included in this retrospective cohort study. The GSS was defined as the time from diagnosis of GVHD (for acute and chronic GVHD separately) until death from a GVHD-related cause, including organ dysfunction directly related to GVHD and infection in the setting of GVHD and immunosuppressive treatment. The GSS in relation to the HCT-CI was analysed using the Cox proportional hazard regression model. The GSS was plotted using the Kaplan-Meier method and the Log-rank test was used for comparison.
Results: The incidence of all grades of acute GVHD and grade 2-4 acute GVHD was 68.7±2.1% and 54.9±2.3%, respectively. The incidence of chronic GVHD by the NIH consensus criteria was 72.9±2.8%. With a median follow-up duration of 24 months among survivors after a diagnosis of GVHD, the 2-year rates of acute GSS (aGSS) and chronic GSS (cGSS) were 60.7±2.9 and 74.6±2.7%, respectively.
Univariate analysis demonstrated that the HCT-CI score as a continuous variable was prognostic for aGSS (p=0.001, HR 1.198, 95% CI [1.082-1.325]), showing that an increase in the HCT-CI score by 1 resulted in an increase in mortality by 20%. However, for cGSS, there was only borderline statistical significance with a p-value of 0.068 (HR 1.130 95% CI [0.991-1.289]).
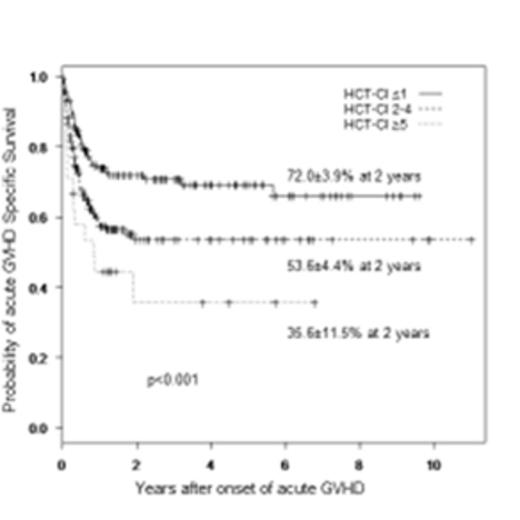
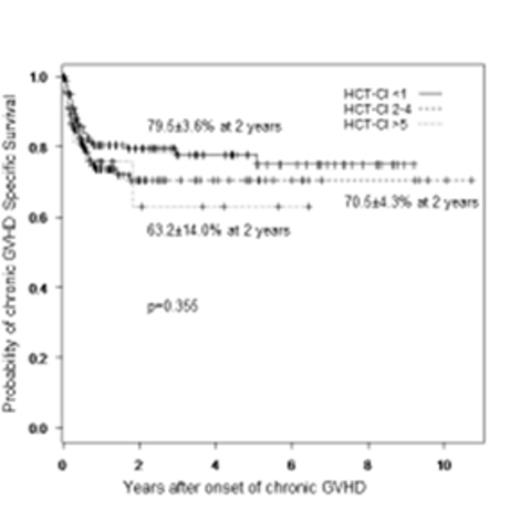
Patients were divided into 3 groups according to their HCT-CI score: 0-1(n=232, 42.9%), 2-4 (n=267, 49.4%) and ≥5 (n=42, 7.8%). The HCT-CI was able to stratify patients in relation to aGSS (p=0.001): The 2 year aGSS rate was 72.0±3.9% in those with an HCT-CI of 0-1 (n=148), 53.6±4.4% with an HCT-CI of 2-4 (n=173), and 35.6±11.5% with an HCT-CI of ≥5 (n=25). In contrast, no correlation was found with cGSS among the 3 groups (p=0.355). The 2 year cGSS rate was 79.5±3.6% in patients with an HCT-CI of 0-1 (n=141), 70.5±4.3% with an HCT-CI of 2-4 (n=149), and 63.2±14.0% with an HCT-CI of ≥5 (n=24).
A multivariable analysis was performed to confirm the HCT-CI score as an independent prognostic factor for GSS, accounting for the following covariates: age, donor type, source of stem cells, and severity of acute GVHD (grade 3-4 vs others) and chronic GVHD (NIH global score mild, moderate and severe). The HCT-CI was found to be an independent risk factor for aGSS (p=0.016, HR 1.15, 95% CI [1.03-1.3]), but not for cGSS (p=0.80, HR 1.02, 95% CI [0.84-1.2]).
Conclusion: Patients undergoing allogeneic HCT with significant comorbidities prior to transplant demonstrated by a higher HCT-CI have a shorter GSS. This finding is only significant for survival following acute GVHD (i.e. acute GSS), but not for chronic GVHD. This study suggests that the HCT-CI score may provide additional prognostic information in the assessment of the risk of acute GVHD related outcomes but not chronic GVHD outcomes, and that the assessment of HCT-CI score prior to HCT may be useful in risk adaptive preventive and treatment strategies for GVHD.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal