Abstract
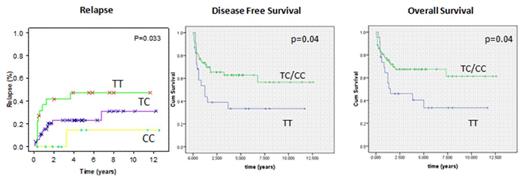
Allogeneic hematopoietic stem cell transplantation (HSCT) using sibling donors is a life-saving intervention for patients with hematological malignancies. It is recognized that numerous genetic factors in both patient and donor play a role in outcome. TGF beta 1 is a member of a highly pleiotrophic family of growth factors involved in the regulation of numerous immunomodulatory processes. Several functional polymorphisms have been identified in TGF-B1 gene, such as a single nucleotide polymorphism (SNP) at codon 10 of exon 1. We have previously published significant impact of this SNP on unrelated donor (UD) transplant outcome, predominantly on Non Relapse Mortality (NRM) and acute Graft-vs.-Host-Disease (aGVHD). To date there are no published data in large sibling donor HSCT cohorts that analyze survival outcomes. We have hypothesized TGF-B1 SNP may influence the outcome of sibling donor HSCT similarly to UD. One hundred and sixty six patient/donor pairs who underwent a sibling donor HSCT in our centers were genotyped for the presence of a SNP at codon 10 (rs1982073) by an allele-specific PCR. The transplant took place between January 2000 and March 2014 and the median follow up time was 4.4 years. Median age was 33 years and 59% were male. The prevalent diagnoses were acute myeloid leukemia 54 (32%), acute lymphoid leukemia 33 (20%), lymphoproliferative disorders 24 (14%), myelodysplastic syndrome 21 (13%), myeloproliferative neoplasm 9 (5%), and 42% were in early stage. Myeloablative conditioning regimens were used in 58% of transplants; the source was PBSC in 93.3% of the patients. The patients' observed SNP frequencies were TT 22%, TC 56% and CC 22%, and for the donors were 25%, 57% and 18% respectively. No significant impacts were observed in the full cohort analysis. When we analyzed the myeloablative cohort significant differences were founded. Wild-type donors (TT) experienced a significant increase in relapse incidence compared to other genotypes (1-3 years TT 37-41% vs. TC 15-23% vs. CC 0-0%, Gray's test p=0.01), with a significant decrease in disease free survival (DFS) (1-3 years TT 53-39% vs. TC/CC 73-65%, log-rank p=0.04) and overall survival (OS) (1-3 years TT 64-46% vs. TC/CC 77-67%, log-rank p=0.04) (figures). No differences in terms of NRM were founded. We conclude that in sibling donor-HSCT TGF-B1 wild-type donors might be associated with an increase in relapse and subsequent decrease in DFS and OS. These results should be confirmed in larger series. Identification of these SNPs pre-transplant will allow for transplant conditioning and immunosuppression regimens to be tailored to the individual patient, as well as assisting in the most appropriate choice of donor.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal