Abstract
INTRODUCTION: Cyclophosphamide (CTX) is an alkylating agent of the nitrogen mustard type, regarded as one of the most potent immunosuppressive drugs available. An activated form of this drug, phosphoramide mustard, alkylates, or binds, to DNA. Its cytotoxic effect is mainly due to cross-linking of strands of DNA and RNA, and to inhibition of protein synthesis. Its has been shown that CTX suppress T-helper cell functions with prolonged reduction of B cells due to the slower rate of recovery of B lymphocytes from an alkylating agent. As in many chemotherapeutic drugs, a major hindrance to the effectiveness of cyclophosphamide in long term leukemic therapy is the target cells subsequent development of resistance against the drug.
OBJECTIVE: The main objective of the research was to implement the determinations of the ex vivo resistance to cyclophosphamide profile and to identify the genetic profile for pediatric patients with acute leukemias.
METHODS: In order to determine the ex vivo drug resistance profile, MTT cytotoxicity assay was performed on mononuclear cells. Gene expression profiles were prepared on the basis of cRNA hybridization to oligonucleotide arrays of the human genome (Affymetrix) for 51 patients with ALL and 16 patients with AML. Hierarchical clustering, assignment location and biological function were performed during the correlation analysis for identified probe sets. Verification of the relative expression level of selected genes was carried out by real time PCR. In order to gain new insights into the molecular mechanisms involved in cyclophosphamide resistance, we performed array-based comparative genomic hybridization (aCGH) on a series of 24 primary acute leukemias, using a SurePrint G3 Human CGH Microarray, 8x60K (Agilent). Data was analyzed by bioinformatics tools: Partek Genomics Suite, PANTHER tools, KEGG Pathway, Agilent Feature Extraction & CytoGenomics.
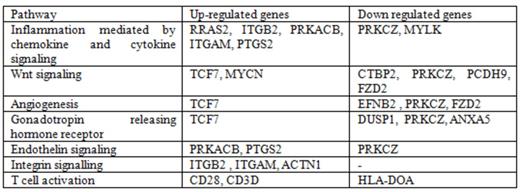
RESULTS: Based on the global expression profile and LC50 values we found, that cyclophosphamide and bortezomid are demonstrating the most different resistances profile, in relation to 20 antileukemic drugs analyzed in the entire research. We observed a multitude of differentially expressed genes, e.g., AKR1C3 (Fold Change=2,81, p-value=0,049), ANXA1 (FC=3,04, p=0,011), BCL2A1 (FC=2.69, p=0,019), SERPINA1 (FC=2.12, p=0.014), DHRS7 (FC=2.13, p=0.005), PCDH9 (FC=-4.58, p=0.015), TTC28 (FC=-2.25, p=0.033) and DUSP1; (FC=-2.91, p=0,002). We assigned the differentially expressed genes to functional pathways (Table 1).
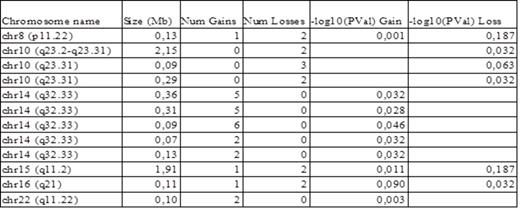
Table 2 shows consistently amplified and deleted regions in acute leukemias samples. A 0.29-Mb stable deleted region involving 10 genes was detected at 10q23.31. Among the affected genes are copy number variants in the IFIT3 gene (interferon-induced protein with tetratricopeptide repeats 3), which regulates cell migration, proliferation and signaling. IFIT3 exhibit an antiproliferative activity via the up-regulation of cell cycle negative regulators CDKN1A/p21 and CDKN1B/p27. Simultaneously we have found for this gene, a significant decrease of mRNA expression of in resistant cells (FC=-2.15, p=0.023).
Panther pathway analysis of differentially expressed genes (cutoff = 2 relative expression change).
Panther pathway analysis of differentially expressed genes (cutoff = 2 relative expression change).
CONCLUSION: Our work delineated genes with diferentiated expression, recurrent copy number changes and revealed novel amplified loci and frequent deletions in resistant to cyclophosphamide in children leukemias, which may guide future work aimed at identifying the relevant target genes. In particular, deletion seems to be a frequent mechanism of inactivation of the IFIT3 gene. Among the candidate genes of resistance may also be included: ANXA1, SERPINA1, TCF7 and BCL2A1.
This study was supported by Grant from the National Science Centre No. DEC-2011/03/D/NZ5/05749.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal