Abstract
Introduction:B-cell maturation antigen (BCMA) is a tumor necrosis factor receptor family member that is expressed on normal and malignant B-cells, including those from patients (pts) with multiple myeloma (MM). Our group has recently shown that this protein is present in the serum of MM pts, and preliminary findings from our group suggested that its levels may correlate with their clinical status and overall survival (OS; Sanchez et al. Brit J Haematol 2012). We now have analyzed the relationship between serum BCMA levels and monoclonal (M)-protein levels as well as the relationship of BCMA to response status, progression-free survival (PFS) and OS in a large cohort of MM pts including those with nonsecretory disease (NSD).
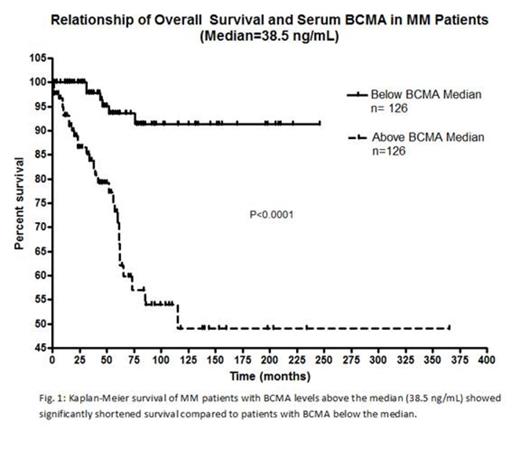
Methods:Two hundred fifty-two MM pts were evaluated. Enzyme-linked immunosorbent assay (ELISA) was used to determine serum BCMA levels (R&D Systems). The Kruskal-Wallis Test was used to assess the correlation between serum BCMA levels and clinical status, and Dunn’s posttest was used to assess differences between clinical status groups. Kaplan-Meier analysis and multivariate Cox regression models were also used. Kaplan-Meier survival of MM pts was determined from the time of initial serum BCMA measurement to death or the date of last follow-up. PFS of MM pts was evaluated from the time of initial serum BCMA measurement to date of first disease progression. Cox-proportional hazards regression was utilized to determine the predictive influence of serum BCMA and various other factors including age, creatinine, hemoglobin, ISS stage, and bone disease on OS and PFS. P-values less than .05 were considered statistically significant. Changes in serum BCMA levels were correlated with serum M-protein levels for 44 consecutive MM pts during their course of disease. Similarly, BCMA was correlated with bone marrow and PET scan findings for NSD pts.
Results: Serum BCMA levels correlated with the patient’s clinical status at the time of its determination (p<.0001). Specifically, pts with > PR had significantly lower serum BCMA levels (median, 11.69 ng/mL) than those with stable and progressive disease (median, 64.17 ng/mL; p<.001). Changes in serum BCMA levels highly correlated with changes in serum M-protein among 44 consecutive MM pts that had multiple determinations made during their course of disease. Notably, pts with NSD showed a direct correlation between changes in serum BCMA levels and their clinical status as reflected by PET scan and bone marrow findings during their course of disease. For the pts (n=64) for whom PFS was evaluable, it was markedly longer among pts with serum BCMA levels below the median (<21.6 ng/mL) compared to those with levels above the median (p<.0006). Among all 252 pts, OS of pts whose serum BCMA levels were above the median (≥ 38.5 ng/mL) was significantly shorter (5-year, 71%) than among those whose levels were below the median (5-year, 94%; < 38.5 ng/mL; p<.0001). We divided pts into three stages based on their serum BCMA levels: Stage 1 (n=118; < 30 ng/ml), Stage 2 (n=79; >30-140 ng/mL) and Stage 3 (n=55; > 140 ng/mL). Pts in Stage 1 had a longer OS (5-year, 95%) compared to pts in Stage 2 (5-year, 72%; p < 0.0002) while pts in Stage 2 had a longer OS than pts in Stage 3 (5-year, 60%; p < 0.0109). We determined the relationship of OS to serum BCMA level, age, serum creatinine, hemoglobin, ISS stage, and bone disease through Cox proportional-hazards regression. In the multivariate regression analyses, serum BCMA levels significantly correlated with only OS (p<.0003). In contrast, age, bone disease status, serum creatinine, hemoglobin, and ISS staging did not correlate with OS. Lastly, serum BCMA was independent of ISS staging and serum creatinine levels.
Conclusion:The results of this study demonstrate that BCMA is a novel serum marker that can be used to follow the course of disease for MM pts. The level of this serum protein is also correlated with clinical status and predicts their PFS and OS. It also provides MM pts with NSD a new potential way to follow their disease course, which currently requires frequent PET scans and bone marrow exams.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal