Abstract
INTRODUCTION: Chronic myelomonocytic leukemia (CMML) is a myeloid neoplasm that belongs to the category of myelodysplastic syndrome / myeloproliferative neoplasms (MDS / MPN). The International Prognostic Scoring System for Myelodysplastic Syndromes (IPSS) classification and its revised version (IPSS-R) addressed patients with newly diagnosed, untreated MDS and excluded CMML. While numerous investigators have attempted to devise a prognostic risk scoring system for CMML, no system has been generally accepted for this entity. A CMML-specific prognostic scoring (CPSS) system proposed by Such, et al [Blood. 2013; 11;121(15):3005-15] defines 4 different prognostic risk categories for estimating both overall survival (OS) and risk for AML transformation; the alternative version replaces RBC transfusion dependency with hemoglobin levels.
AIM: The aim of the study is to validate the alternative CPSS scoring system on the CMML patient cohort at UT MD Anderson Cancer Center (UTMDACC).
METHODS: The databases of the Department of Hematopathology at UTMDACC were searched for patients diagnosed with CMML presenting from 2005 to 2012. Cases were classified by WHO 2008 criteria. Inclusion criteria were: confirmed diagnosis of CMML, age > 18 years, persistent absolute monocyte count >1 × 109/L, marrow blasts < 20%, peripheral blood blasts < 20%. The alternative CPSS score was calculated as a function of WHO subtype, FAB subtype, CMML-specific cytogenetic risk classification, and hemoglobin score. Cox proportional hazards regression was used to model overall survival and time to AML progression from date of diagnosis. For time to AML progression, patients who did not experience AML progression were censored at their date of death or last follow-up. Kaplan-Meier curves were used to estimate survival and the log-rank test was used to test for significant differences by CPSS score. All statistical analyses were performed using SAS 9.3 for Windows.
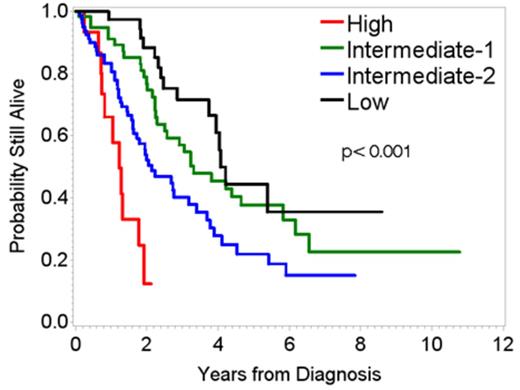
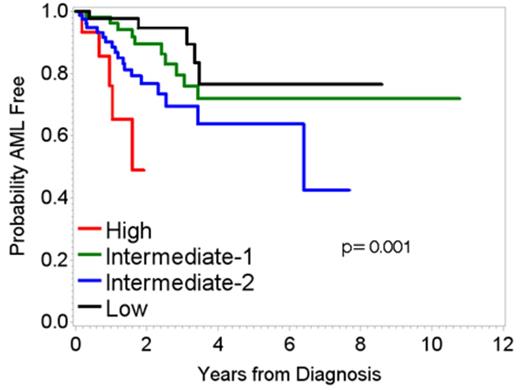
RESULTS: Two hundred and three patients with newly diagnosed, untreated CMML were identified in the clinical databases. These included 132 males and 71 females; median age was 70 (range 55-80) years. 149 had CMML-1 and 54 had CMML-2. A total of 107 deaths and 38 progressions were observed. The median (range) follow-up time for all patients was 1.9 (2 days-10.8) years. The variables that compose the alternative CPSS (WHO subtype, FAB subtype, CMML-specific cytogenetic risk classification, hemoglobin) as well as a description of how the score is calculated are given in Tables 1-2. In univariate Cox models, the alternative CPSS score was a significant predictor of both OS and time to AML progression (Type III p-values <.0001 and 0.0037, respectively). Median survival times for OS were 4.07, 3.32, 2.14, and 1.23 years in the low, intermediate-1, intermediate-2, and high risk groups, respectively. Since less than half the patients progressed, the median time to AML progression could not be estimated for all groups but was 6.40 and 1.60 in the intermediate-2 and high risk groups, respectively. Overall, the alternative CPSS score was highly predictive of both OS and progression free survival (PFS) and clearly delineated the patient risk groups in this sample.
CONCLUSIONS: These data reinforce the validity of the alternative CPSS and serve as an additional validation cohort.
Alternative CMML-specific prognostic scoring system (CPSS) score criteria
| Variable . | Each level assigned the following value (sum to get the composite CPSS score): . | ||
|---|---|---|---|
| 0 . | 1 . | 2 . | |
| WHO subtype | CMML-1 blasts (including promonocytes) <5% in the PB and <10% in the BM | CMML-2 blasts (including promonocytes) from 5% to 19% in the PB and from 10% to 19% in the BM, or when Auer rods are present irrespective of blast count | — |
| FAB subtype | CMML-MD (WBC <13 × 109/L) | CMML-MP (WBC ≥13 × 109/L) | — |
| CMML-specific cytogenetic risk classification* | Low | Intermediate | High |
| Hemoglobin | ≥10 g/dL | <10/dL | |
| Variable . | Each level assigned the following value (sum to get the composite CPSS score): . | ||
|---|---|---|---|
| 0 . | 1 . | 2 . | |
| WHO subtype | CMML-1 blasts (including promonocytes) <5% in the PB and <10% in the BM | CMML-2 blasts (including promonocytes) from 5% to 19% in the PB and from 10% to 19% in the BM, or when Auer rods are present irrespective of blast count | — |
| FAB subtype | CMML-MD (WBC <13 × 109/L) | CMML-MP (WBC ≥13 × 109/L) | — |
| CMML-specific cytogenetic risk classification* | Low | Intermediate | High |
| Hemoglobin | ≥10 g/dL | <10/dL | |
WBC: white blood cell
* CMML-specific cytogenetic risk classification; low: normal and isolated –Y; intermediate: other abnormalities; and high: trisomy 8, complex karyotype (≥3 abnormalities), chromosome 7 abnormalities
Alternative CPSS: scores used for predicting likelihood of survival and leukemic evolution in individual patient with CMML
Risk group . | Overall CPSS score . |
|---|---|
| Low | 0 |
| Intermediate-1 | 1 |
| Intermediate-2 | 2-3 |
| High | 4-5 |
Risk group . | Overall CPSS score . |
|---|---|
| Low | 0 |
| Intermediate-1 | 1 |
| Intermediate-2 | 2-3 |
| High | 4-5 |
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal