Abstract
[Background] Approximately 10-20 % of the patients with myelodysplastic syndrome (MDS) are known to be complicated by autoimmune or inflammatory disorders (ADs) such as vasculitis. However, most of the reports on such MDS were published before 2000, in which the diagnosis of MDS was made with previous criteria; about 20% (range 9-43%) of the patients in these reports may not be diagnosed as MDS with the present criteria. In addition, many of these reports do not offer sufficient information on cytogenetic analysis, a presently known critical factor that affect pathophysiology of MDS. These facts could make difficult to discuss its characteristics, prognosis and treatment options. Therefore, we made a detailed retrospective analysis on clinical features and treatment outcomes of MDS complicated by ADs based on more recent knowledge.
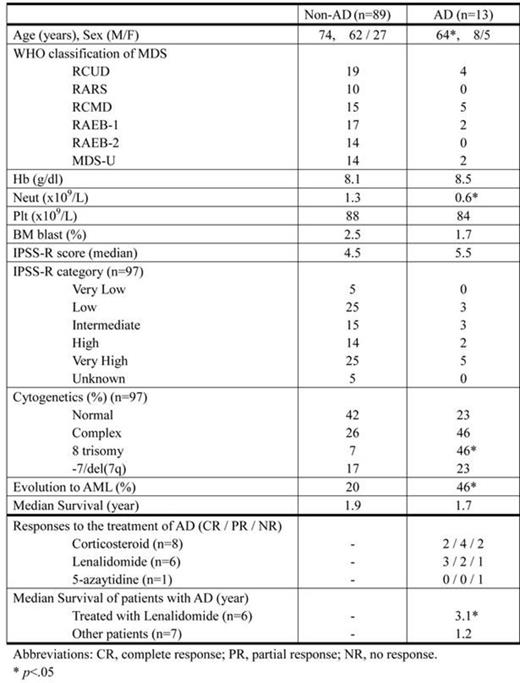
[Results] A total of 102 Japanese patients with MDS (70 males and 32 females, median age of 73), diagnosed between June 2007 and June 2014, were evaluated. The diagnosis was made with WHO (2008) classification. Bone marrow G-band chromosome analysis was available in 95 % of the patients. "Very High" risk category of IPSS-R criteria comprised 29% of the patients. As summarized in Table 1, 14 episodes of AD were observed in 13 (13%) patients; 4 with Sweet syndrome, 2 each with Bechet like symptoms, interstitial pneumonia, large vessel vasculitis and myelitis, and 1 each with HPS and seronegative arthritis. As in the previous reports, the patients who developed ADs (AD group) were characterized by younger age and higher frequency of complex cytogenetics compared with those who did not (non-AD group). In addition, patients of AD group showed lower neutrophil count and higher frequency of trisomy 8 (p=.034 and <.01, respectively). Of note, despite no significant difference in median IPSS-R score, the progression rate to AML in AD group was more than two-times higher compared with non-AD group (p=.01). Survival rates were not significantly different between two groups.
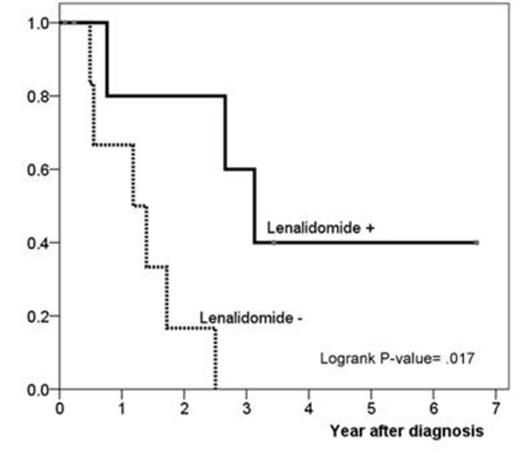
Corticosteroids were given to 8 patients of AD group and 6 of them (75 %) showed a certain degree of responses. Six patients with relapsed or refractory AD after the steroid therapy were treated with low-dose Lenalidomide (LEN) (10mg/day for 21 days). Interestingly, 5 of them responded to LEN with 3 achieving complete remission. Furthermore, the patients of AD group received LEN showed better survival compared with those treated without LEN (1.2y vs. 3.1y, p=.017) (Figure 1).
[Conclusion] The present observation indicated that MDS with AD may be associated with cytogenetic abnormalities including trisomy 8 and higher progression rate to AML. Of note, LEN might be a possible treatment option for those resistant to steroid therapy.
Clinical features of the patients who were complicated by autoimmune or inflammatory disorders (AD) and those who were not (non-AD)
Clinical features of the patients who were complicated by autoimmune or inflammatory disorders (AD) and those who were not (non-AD)
Comparison of Kaplan-Meier estimates of survival in the presence or absence of Lenalidomide treatment
Comparison of Kaplan-Meier estimates of survival in the presence or absence of Lenalidomide treatment
Nakamae:Novartis: Honoraria, Research Funding, Speakers Bureau, Travel/accomidations/meeting expenses Other. Hino:Nippon Shinyaku CO.,LTD: Research Funding; astellas CO.,LTD: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal