Abstract

Introduction: In adults with Philadelphia chromosome negative (Ph-) acute lymphoblastic leukemia (ALL), the optimal post-remission therapy remains uncertain. Although allogeneic hematopoietic cell transplantation (HCT) in first complete remission (CR1) has become a widely adopted curative strategy, the need for HCT may be supplanted by intensive, pediatric-style chemotherapy regimens. These two approaches have not previously been compared.
Methods: We evaluated the outcomes of 422 related or unrelated donor HCT recipients aged 18-50 years with Ph-ALL in CR1 between 06/2002 and 12/2011 as reported to the CIBMTR. This was compared to a concurrent cohort of 108 Ph- ALL CR1 pts (18-50 years) who received a Dana Farber Cancer Institute (DFCI) ALL Consortium pediatric regimen consisting of intensive, non-HCT therapy. Primary outcome was disease-free survival (DFS). Patients in the DFCI chemotherapy cohort who received HCT in CR1 were censored at the day of HCT. Left-truncated analysis methods were used to adjust time from CR1 to transplant.
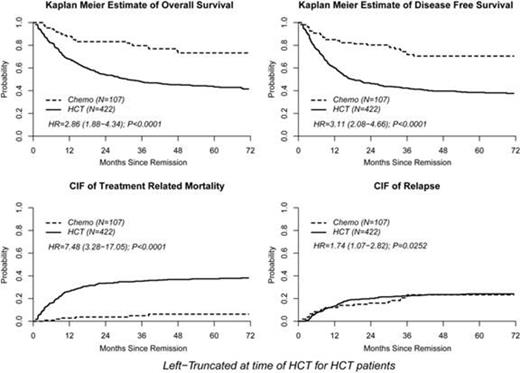
Results: The HCT cohort was older (median age 34 vs. 30 years, p=0.001) and had higher diagnostic WBC counts (median 12x109/L [range <1-515) vs. 8x109/L [1-1424], p=0.001, respectively). The proportion of patients with T –ALL was lower in the HCT cohort (14% vs. 22%, p=0.03), while the incidence of t(4;11)/MLL was similar in both groups (8% vs. 10%, respectively). Of the HCT cohort 396 (94%) underwent myeloablative (MA) conditioning. Donor source was matched related donor in 176 (42%), 8/8 unrelated donors in 168 (40%), and 7/8 (18%) from 7/8 unrelated donors. In univariate analyses (Figure 1) cumulative incidence of relapse at 4 years was similar in both groups (HCT 25% [19-28] vs. chemo 23% [15-32] p=0.97). Two-year treatment-related mortality (TRM) was higher in the HCT cohort (HCT 33% [28-39] vs. chemo 4% [1-8], p<0.0001). At 4 years, DFS was superior in the chemo cohort (HCT 40% [35-45] vs. chemo 71% [60-79], p<0.0001). Four year OS also favored chemo (HCT 45% [40-50] vs. chemo 73% [63-81], p<0.0001). In multivariable analysis, independent factors predictive of treatment failure (relapse or death) were HCT (HR 3.11 [2.08 – 4.66], p<0.001) and the presence of CNS disease at diagnosis (HR 1.56 [1.03 – 2.38], p=0.04). The sole factor associated with poorer OS was the administration of HCT (HR 2.86 [1.88 – 4.34], p<0.0001). The favorable OS with chemo was maintained when restricting the HCT cohort to those recipients with related donors or fully matched (8/8) unrelated donors and those whose time from diagnosis to CR1 was <8 weeks (HR 2.14 [1.36-3.35], p=0.001). Similar outcomes were seen when restricting the HCT cohort to those who achieved CR1 < 8 weeks from diagnosis and received myeloablative conditioning.
Conclusion:In this comparison of two cohorts of younger Ph- negative adults in CR1, post-remission therapy with an intensive, pediatric-inspired, chemotherapy-based regimen conferred a survival advantage when compared to allogeneic HCT. The high TRM associated with HCT is a major factor in determining outcomes after HCT. In an era of increasing adoption of pediatric regimens for adults with Ph- ALL, allogeneic HCT may no longer be required for the majority of patients who achieve CR1. These data support the need for randomized controlled studies in Ph- ALL comparing pediatric-inspired non-HCT regimens to allogeneic HCT-based therapy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal