Abstract
The current definitions of red-cell transfusion dependence (TD) for MPN-associated MF are based on expert opinion. The optimal definition of TD, and its impact on the natural history of MF is not well studied. We evaluated the impact of two definitions of red-cell TD on the natural history of 306 patients (pts.) with WHO/IWG-MRT-defined primary MF (PMF, n=202, 66%), post-polycythemia vera MF (PPV-MF, n=45, 15%) or post-essential thrombocythemia MF (PET-MF, n=59, 19%).
Red-cell TD was defined according to IWG-MRT 2006 criteria (Tefferi et al, Blood, 2006), and on the results of the expert consensus RAND-Delphi panel (Gale et al, Leukemia Research, 2011). The IWG-MRT criteria require patients to have received ≥2 Units (U) packed red blood cells (PRBC) in the preceding 28 days for hemoglobin (Hb) <85 g/l. On the other hand, the more stringent Gale definition requires patients to receive ≥2 U of PRBC per month over 3 months without any specification for the Hb level. Patients were evaluated for disease risk stratification according to dynamic international prognostic scoring system (DIPSS), co-morbidities according to ACE-27, and red-cell TD at their first presentation to Princess Margaret Cancer Center or diagnosis.
The study cohort was divided in 4 groups (gp.): Non-transfusion dependent (NTD) pts. with Hb ≥100 g/dl (gp1, n=156, 51%); patients with Hb <100 g/dl, but no transfusion in preceding 12 weeks (gp2, n=65, 21%); pts. qualifying IWG-MRT 2006 criteria of TD, but not qualifying Gale definition (gp3, n=41, 13%); and pts. qualifying the Gale definition of TD (gp4, n=44, 14%). There was no significant difference among the 4 groups with relation to age, disease distribution (primary vs. secondary), cytogenetics, blasts%, and ACE-27 co-morbidity scores. There was significant difference in the gp1, gp2, gp 3, and gp4 in relation to constitutional symptoms (35% vs. 45% vs. 46% vs.64%, p=0.006), median WBC count (x109/L) (11.5 vs. 8.3 vs. 6.8 vs. 6.5, p<0.0001), platelets (x109/l) (317 vs. 154 vs. 124 vs. 127, p<0.0001), and Int-2/high DIPSS (24% vs. 82% vs. 90% vs. 82%, p<0.0001).
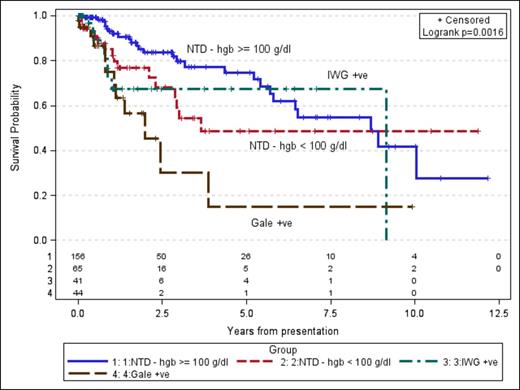
In a univariate analysis, probability of survival among the 4 groups at 3-years was 80%, 55%, 68%, 30%, respectively (Fig 1, p=0.0016). No difference in leukemic transformation was observed among the 4 groups (p=0.68). In a multivariate analysis, after adjusting for DIPSS and co-morbidity scores, hazard ratios among the gp2, gp3, and gp 4 were 1.58 (95% CI 0.78-3.19, p=0.21), 2.17 (95% CI 0.88-5.34, p=0.09), 2.82 (95% CI 1.29-6.16, p=0.009) in comparison to gp 1 (ref. group). There was no significant difference between NTD patients with Hb <100 vs. TD patients according to IWG-MRT 2006 criteria, but not meeting Gale Criteria (p=0.47). DIPSS was the only other independent prognostic factor for survival.
Our study shows the independent prognostic impact of TD on survival defined according to Gale criteria, but not according to previous IWG-MRT 2006 definition, which does not meet Gale criteria. No impact of anemia or TD was observed on leukemic transformation.
Survival in 4 groups according to Hb levels and transfusion needs
Survival in 4 groups according to Hb levels and transfusion needs
Schuh:Celgene: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal